Today is another great day. Been very busy lately, regardless, I will always make out time to drop interesting gist here. I wish to discuss a very important wave of advancement that has been seen in the field medicine. Our focus today will be on cancer but this time, I intend to go deeper to explore what has happened so far.
Reading this article will bring you up to speed on how far research has gone to finding long lasting solution and cure to cancer. From time immemorial, it is believed that cancer has no cure, but in our present dispensation, it is a different thing now. Join me as I unveil very interesting findings that can be applied in cancer cure.
It is no longer news that cancer is one of the disease that has been plaguing humans for a very long time. It doesn't matter who you are or what you are, it affects anyone and at any time. Cancer is simply an abnormal growth of cells in any tissue or organ. Cancer is a growth that is deviating from the control of the body.
Cancer cells grow independent of the physiologic control of the body. They are unregulated and as such, grow with no restrictions. Cells in the body are subject to regulatory mechanism and checkpoints during cell division but in a situation where these check points and regulators are absent or altered due to one reason or the other, for example, due to mutation (an alteration in the genetic make up of a living organism) , this results to uncontrolled division and growth.
Depending on the stage of the cancer and type of the cancer, some can migrate from one part of the body to the other and this process is known as metastasis. Metastatic cancers are more deadlier than normal type of cancers because of their ability to invade normal tissues and cells.
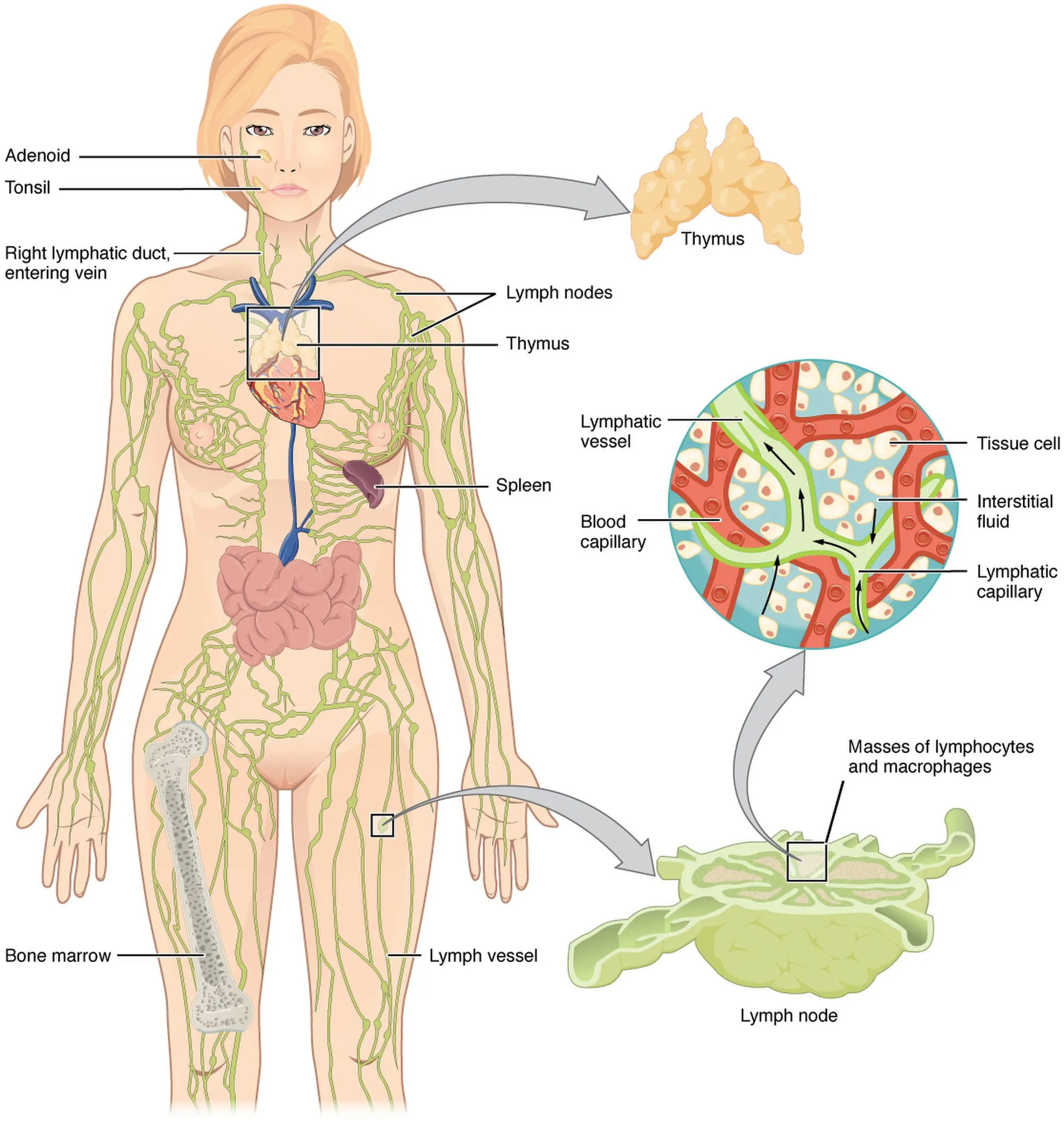
They tend to thrive more through the lymphatic system (a drainage system in the body that is responsible for the drainage of fluids from all the organs in the body back into the blood vessels) and this can be seen more to be associated with breast cancers. The lymphatic system even though enables drainage from all tissues, it also plays a significant role in conferring natural immunity in humans and this typically occurs in the lymph nodes.
For example, a typical lymphatic tissue that play role in immunity is the thymus. The thymus is the major organ that is responsible for the production of T-cells aka lymphocytes in the body. Lymphocytes are group of white blood cells that primarily play the role of offering protection in humans. The ability of immunity cells to know and differentiate between the cells of its own and that of other invading pathogens is gained in the thymus. Any cell or substance capable of causing harm and that is not of the body, is destroyed.
The thymus trains these lymphocytes (aka T-cells) so well that after maturation, they are able to mount a defensive attack on any foreign body that may try invading the body system. So in essence, you can simply say that the thymus is the school for lymphocytes and after graduation, they return to the general body system to do their job of protection.
Usually when the body is invaded by foreign substance, the body responds through the process of mounting immune response by producing antibodies against the invading substance. This process might take a little time and it is usually accompanied with signs and symptoms like headache, raised body temperature, loss of taste etc. At beginning of the immune response, a special type of plasma cells produce B cells that differentiate into Memory B-cells.
Memory B cells circulate in the blood stream in a quiescent state, sometimes for decades. Their function is to memorize the characteristics of the antigen that activated their parent B cell during initial infection such that if the memory B cell later encounters the same antigen, it triggers an accelerated and robust secondary immune response. Memory B cells have B cell receptors (BCRs) on their cell membrane, identical to the one on their parent cell, that allow them to recognize antigen and mount a specific antibody response.
The memory cells keeps track and record of any foreign substance that invaded the body. While this is happening, the body also will produce antibodies to mount the attack on the foreign body. All this are done in a bid to prepare the body to fight the invading substance on subsequent exposure. On another attack, it will waste no time destroying such substance.
A cancer cell that is growing in one of the breast can infiltrate the other easily through the lymphatic system. This is one of the reasons a diseased breast is immediately cut off before a cancer matures and affects the second breast, this occurs mostly in women. You might be wondering what connection does the human immunity has with cancer cells. There is a connection and this was taken advantage of in the development of new targeted therapy for cancer treatment. Read along, you will get a better understanding.
Cancers cells have high regenerative ability and they even have a way of producing more blood vessels through process known as angiogenesis. They do this because in a normal cell, supply of various minerals and nutrients for growth is under regulations in order to avoid issues. Cancer cells bypass this regulations and absorb more nutrients to meet up with their high metabolic rate as evident in proliferation (multiple division and growth). If the regulations where allowed, they would probably be starved to death, hence why they either allow more nutrients absorption or produce more blood vessels.
Cancerous cells are more effectively removed from tissues in its totality through surgery. Surgery though might be more invasive than using chemotherapy (use of drugs for treatment of cancer), is one of the way to remove cancerous growths provided they are not highly invasive. For treatment to be successful, most cancers are better detected and removed at their early stages. Failure to do this, death is certain and inevitable.
Advancement and research so far in finding ways to conquer cancers have to a reasonable extent yielded positive results from all indications and reports. But most of this techniques are not but without their challenges. Some cancers cells cannot actually be treated through surgery, especially cancers associated with the human blood.
There are basically three types of blood cancers depending on the type of blood cells they affect - leukemia (affects the white blood cells), myeloma (affects the plasma cells that produce antibodies in the body), and lymphoma (affects the lymphocytes such as the T-cell). The human blood cells are microscopic in nature and as such, they are not cells that surgery can be carried out on rather, chemotherapies are favored.
Chemotherapies on the other hand are also not but without consequences, and one of which is the destruction of normal cells. As the drugs target abnormal cells, they lack the ability to identify healthy cells and so in all, they end up destroying non cancerous cells. Now Targeted therapies in cancer treatment using drugs, are aimed at ensuring that only cancerous cells are destroyed without having any effect on the non cancerous cells.
The drive to find solution to this led to the discovery of a technique in cancer treatment known as the Chimeric Antigen Receptor T cell therapy. This technique is actually the first of its kind and from my perspective, will be the best option in cancer treatment haven looked at the previous side effects and consequences associated with older techniques of cancer treatment.
The big question is, what is CAR T-cell therapy all about and how does it work?
Just like we established earlier on in the beginning of this article, the human body immune system is naturally programmed in such a way that, it is able to remember invading pathogens and at the same time fight back subsequently. This ability to remember and clearly differentiate its own body cells from that of other foreign substance, is what is taken advantage of in CAR T-cell therapy.
It is a type of immuno therapy that is employed in the treatment of cancer cases. Every cell in the body has its unique antigen associated with it and through this antigens, the body can differentiate self from non self. These antigens are the linking gates for other molecules and substances to bind. Every antigen correspondence to a unique receptor that binds to it. So in essence, if a substance does not have an identical antigen receptor to a cell, it will not be able to bind. It is more like and lock and key model.
The body raises alarm when it detects foreign antigens, hence triggering immune response through the lymphocytes and specifically, the T-cells. Since T-cells are mainly at the front line of defensive action against intruders, it is logical to incorporate them in the identification of cancer cells.
In a nutshell, CAR T-cell therapy is a simple way of gearing up the human T-cells in confronting and destroying cancer cells. Have you now seen the connection between the cancer cells and immunity? There more, read on.
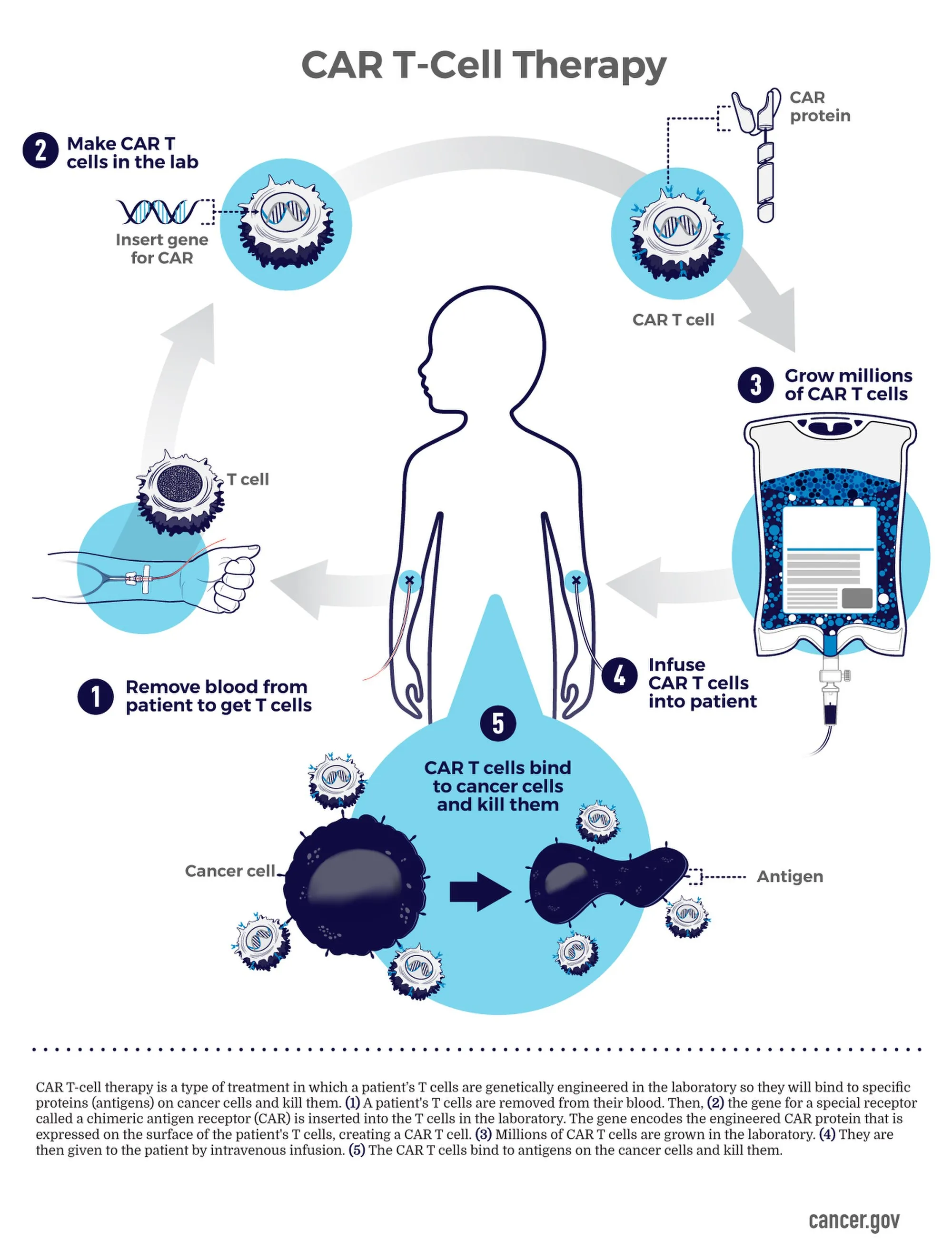
CAR T-cells are genetically modified T-cells that are specifically designed to attack cancer cells in the body. They are made to locate any cell that is cancerous and totally eliminate them from the body. So the use of these genetically modified T-cells in the treatment of cancer disease, is what is referred to as Chimeric Antigen Receptor T cell therapy. This brings us to the question, how is this done?
Stages of Chimeric Antigen Receptor T cell therapy
The process is quite simple not so much complicated for a layman to understand. The only area where I would term complex, is the genetic modification of the DNA of the T-cells. This i won't be bothering you, since I have not got the chance of having a first hand experience on it. Regardless, the explanation I will give below is enough for basic knowledge.
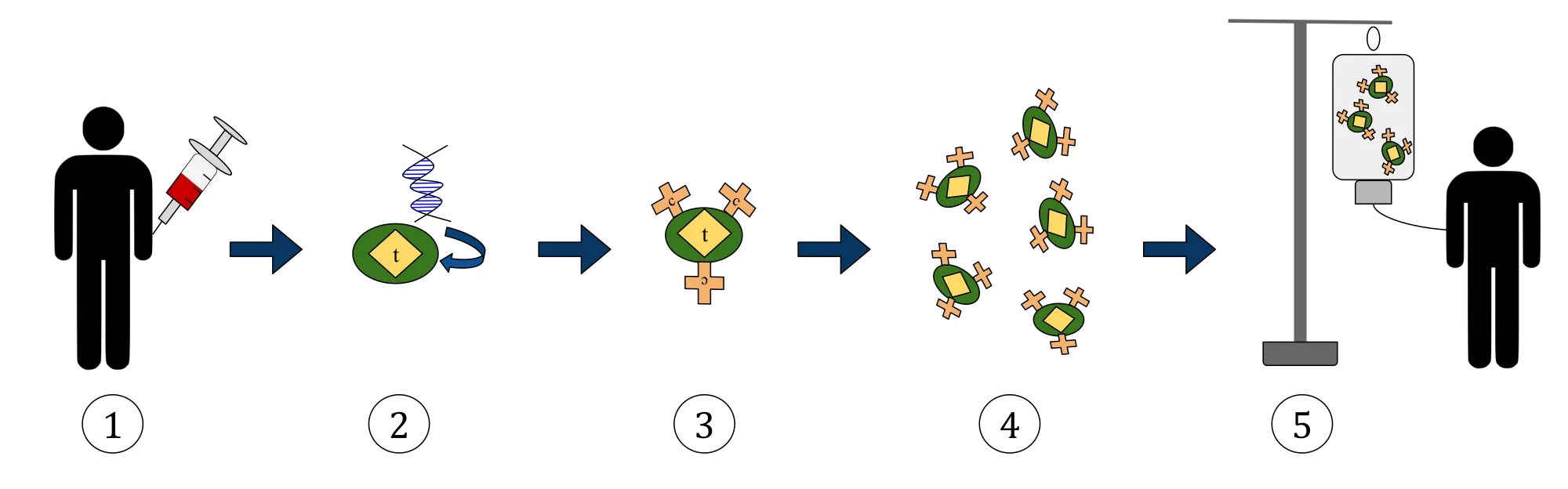
CAR T-cells therapy begins with the extraction of the T-cells from the blood of the patient and then through genetic engineering alter the DNA by infusing a gene for chimeric antigen receptor into it. This receptor when infused helps and gives the T-cells the ability to identify cancer cells in the body of the patient and subsequently destroy them.
Without the infusion of these gene, T-cells cannot destroy cancer cells because cancer cells also exhibit mimickery (they look like normal cells but in the real sense they are not) and are unable to be detected by the immune system as abnormal cells. They have their own antigens to which the immune system cannot bind since we don't have their receptors.
Now that the T-cell have been genetically equipped with the chimeric antigen receptors on their surfaces to specifically attack the cancer cells, they are then harvested and cultured so that they are in abundance in number. Simply out it this way, they are multiplied to numerous numbers and after which they are then harvested and ready to be infused back into the patient.
Importantly, CAR are mostly designed to bind to the CD-19 antigen that is also found on cancer cells aside B-lymphocytes. Any cancer cell that does not express this CD-19 antigen cannot be destroyed since the T-cells won't have any corresponding right receptor for identification, binding and subsequent destruction. In essence, the therapy is not yet applicable to all types of cancer cells.
That notwithstanding, this is a good advancement and efforts being made to win the war between humans and cancer. We only hope that these cancer cells, as crafty as they are, do not at some point, devise a means of circumventing the ability of T-cells in identifying them, since they are notoriously known for breaking rules and never adhering to instructions. They always want to be independent, do what they want, when and however they want, and this is a major concern that needs to be monitored closely.
Well, no matter how they run from us, we will never relent in efforts to combat these cancers. Join the fight by ensuring you eat healthy and avoid exposure to substances that have been termed carcinogenic (substances with the potential of causing cancer).
Until I come your way, stay awesome!
References •CD19 •CAR T Cells: Engineering Patients’ Immune Cells to Treat Their Cancers •Tracking the CAR-T Revolution: Analysis of Clinical Trials of CAR-T and TCR-T Therapies for the Treatment of Cancer (1997–2020) •Chimeric Antigen Receptor T-Cell Therapy •CAR-T Cell Therapies: An Overview of Clinical Studies Supporting Their Approved Use against Acute Lymphoblastic Leukemia and Large B-Cell Lymphomas •CAR-T cell therapy: current limitations and potential strategies •An Overview of the Thymus •The Development and Causes of Cancer •Breast Cancer—Epidemiology, Risk Factors, Classification, Prognostic Markers, and Current Treatment Strategies—An Updated Review
Return from Catching up with the Chimeric Antigen Receptor T-cell therapy for Cancer treatment: Cancer cure is no longer far to cyprianj's Web3 Blog