This article is intended to give a detailed, simplified and easy to understand explanations to what goes on when one is infected with Corona virus, diagnosis and ways to prevent the virus. It also intends to guide the reader on the appropriate use of nose mask and ventilators, principle behind the filtering ability of masks. Its gonna be a long read and as such, this article will be split in two;
First part, about the pathogenesis and pathophysiology of corovirus while second part delves into the use of mask as a personal protective equipment (PPE). This article will be an invaluable compendium for writing detailed literature or assignments on corona virus and how it affects the human body system. I bet, there are a lot you will learn here. Sit tight, enjoy and be informed.
Coronavirus is one heck of a virus that has so far shaked the entire world at large. Since it's outbreak on the 31st of December 2019, it has got the attention of major countries in the world. Some of the worst hit country include China, Italy, USA, Iran etc.
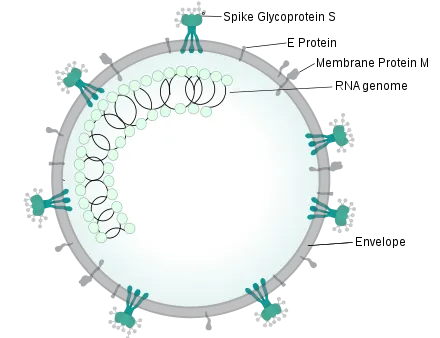
The word COVID-19 simply means Coronavirus -19. The number -19 attached to it simply signifies the year the virus was discovered -2019. The word Corona came about due to the crown-like spikes that covers its outer viral capsid.
Coronavirus particles when released through respiratory droplets are way denser than air and as such cannot be easily blown around by air waves, hence not much of an airbone disease. The droplets produced when an infected person cough, sneezes or talks do not travel more than a distance of about one meter (1m), this is why you are advised to ensure social distancing.
It is a heat labile virus (this simply means that it is easily killed by heat); could this be the reason why the infection rate is more in some cold continents of the world than in tropical regions? That's a topic for another. Simple washing of hands with soap and running water for atleast 20 seconds kills the virus. Let's now go deep into the pathophysiology of the novel virus.
The term pathophysiology simple means the study of all the changes that arise from the body system that is cause by a disease. One gets infected when the respiratory droplets either lands on the mouth, eye or nose.
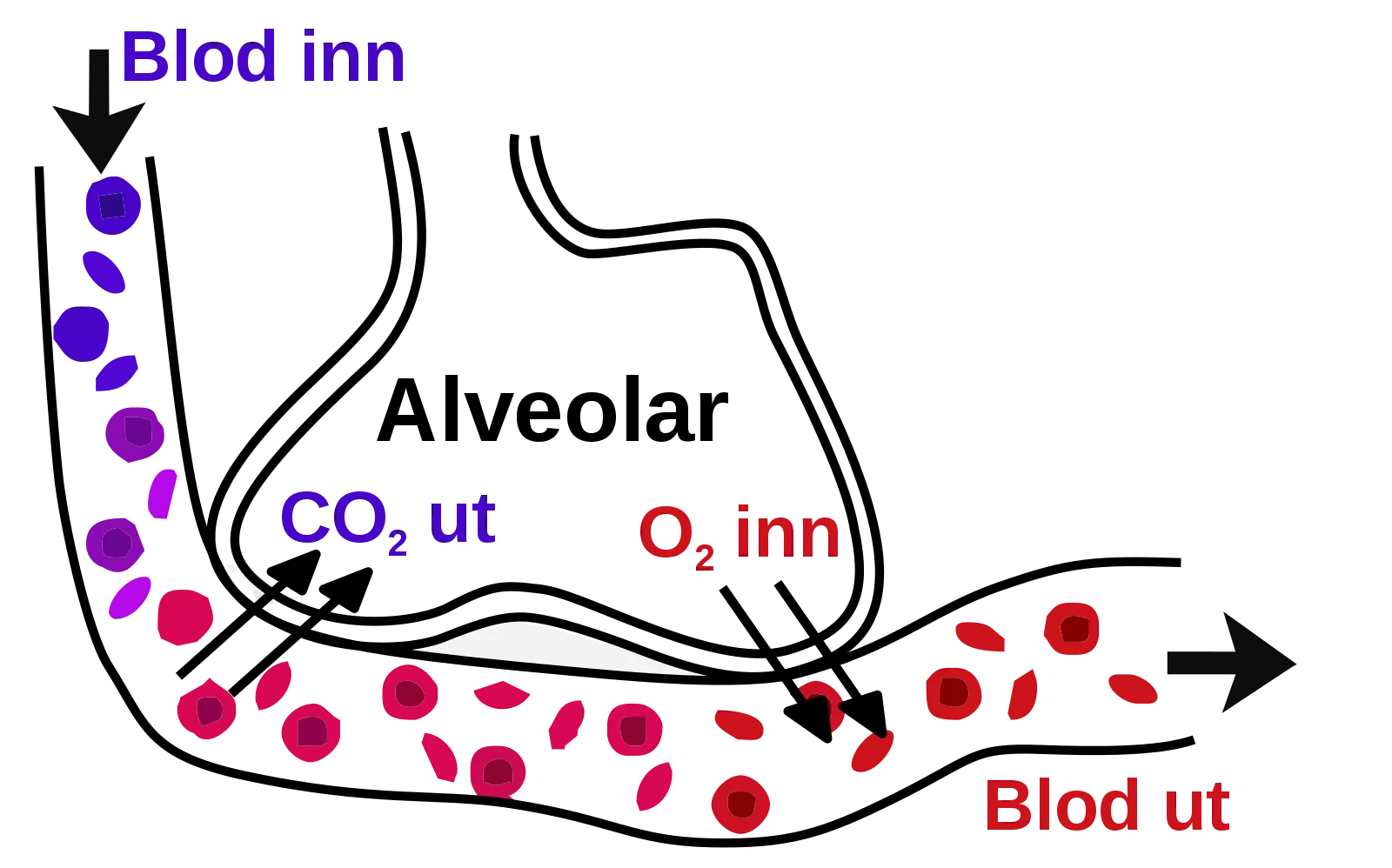
Major route of entry is the mouth or nose or eyes. It is a respiratory virus and damages the lungs, more especially, it loves the alveoli (where gaseous exchange occurs in the lungs). One of the reason why corona virus victims cough is because of the irritant effects the virus has in the respiratory tract.
what happens when they enter the body system
Upon successful entry through any of the earlier mentioned routes, they attach to a very important type of cell in the lungs- the type 2 pneumocyte (cells of the lungs that produces surfactant which functions to reduce surface tension in the lungs thus preventing lung collapse).
It binds to a recetor located on the type 2 pneumocyte using its S-spike. Invariably, if we can produce drugs or vaccines that can make the type 2 pneumocytes resistant to the virus, we could be close to winning the war.
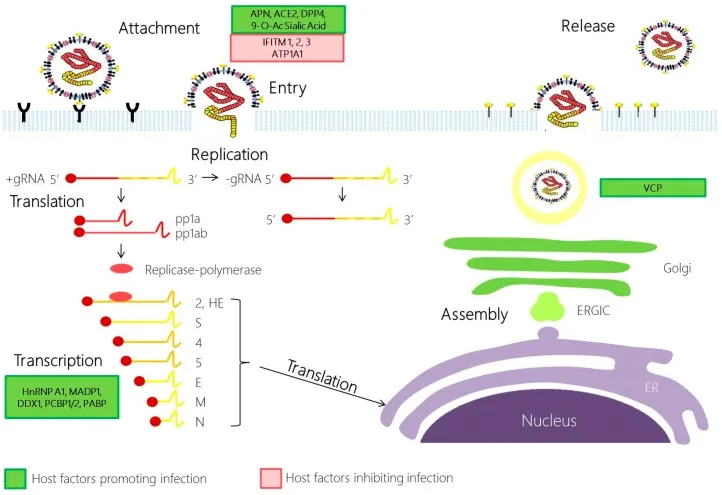
This receptor is known as the Angiotensin converting enzyme receptor (ACE) type 2. This binding enables them to be engulfed into the cell of the pneumocyte. Once inside the cell, it does two things, it releases its positive sense single stranded RNA (+sSRNA) which uses the host ribosome, takes the mRNA from it and converts it into specific proteins (a process known as Translation).
Secondly, by virtue of it being a positive sense virus, it also uses an enzyme called RNA dependent RNA polymerase (RNA-D-RNA Pol). By implication, it takes RNA and produces another RNA i.e it takes that single strand RNA and converts it to more positive sense single stranded RNA.
Using another enzyme called the proteinase that cleaves those specific proteins so that it forms the parent virus and also incorporating the +sSRNA in the process; the cycle begins again The resultant effect is the production of tons of covid-19 virus. This cycle continues to cause damage to the type 2 pneumocytes by the virus.
How the pneumocytes respond to attack
The pneumocytes respond to the damage by releasing inflammatory mediators that are detected by the lung macrophages. These macrophages inturn respond by releasing inflammatory cytokines (proteins released whenever there is an inflammatory condition or injury) such as interleukin1, 6, and tumour necrotic factor alpha. These inflammatory cytokines cause the endothelial cells to dilate thereby increasing capillary permeability (makes the blood vessels more porous)
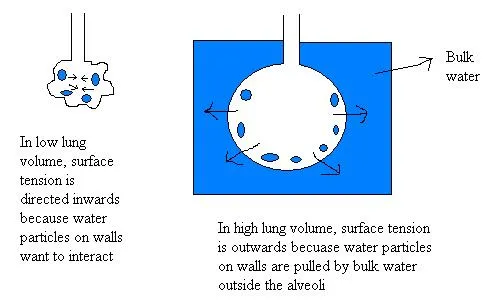
Increased capillary permeability allows fluids like plasma to enter the alveoli and subsume or drown out the surfactant. Remember the surfactant has a very important role to play in the lungs and which is to decrease surface tension. As the surfactant decreases, there is a resultant increase in surface tension.
Pressure and surface tension role in the lungs
If you would recall Laplace law in physics that talks about pressure and surface tension,
"It states that increased pressure causes two times (2×) an increase in surface tension divided by the radius"
So increased surface tension causes increased pressure and ultimately leading to alveoli collapse (this is why patients with Corona virus disease find it very difficult to breath (dyspnea) once the alveoli has collapsed, they will need to work extra hard to breathe).
Since gaseous exchange is not so possible anymore, it leads to a condition known as hypoxemia (low level of oxygen in the blood). I am sure you know that it is a very dangerous situation that can lead to coma. Hope you are now getting to fully understand how this deadly virus operates.
Now the problem does not end there, remember those inflammatory cytokines that were released by the pneumocytes in response to the virus invasion, remember? Good, guess what, these cytokines will attract a type of white blood cell known as the neutrophils ( usually released in cases of viral infections).
What they do is to try and destroy those viruses that are attached to the type 1 pneumocytes (play significant role in gaseous exchange) and type 2 pneumocytes. The big question is at what cost? as they're trying to eliminate or kill the covid-19 viruses, they also end up damaging the pneumocytes and what happens at the end of the day; it only gets worst because when they damage the type 2 pneumocytes, surface tension increases leading to alveoli collapse and if they damage the type one 1 pneumocytes, gaseous exchange becomes a very big problem.
The whole event leads to a condition known as lungs consolidation, a situation where there are deposits and slugs of pneumocytes, inflammatory mediators, neutrophils etc deposited or clustered within the alveoli thus making it much more difficult to breathe.
Why the fever?
You may want to ask why they also feel increased body temperature (fever). Ask no more, the answer is here. Remember the inflammatory cytokines, especially the interleukin1 and 6; now when they are released in very large amount, they travel through the blood and get to the brain.
On getting to the brain, they stimulate the hypothalamus (the heat center) to release some type of prostaglandins such as PGE-2 which has the ability of reset the human body system's thermostat, this ultimately leads to fever (increased body temperature beyond normal =/>100.4 degree F).
Resultant drop in partial pressure effect
Another thing I want to draw your attention to, is low partial oxygen pressure (Po2). Remember they become hypoxemic (low oxygen level). Now in a situation where you have a reduced partial oxygen pressure, in response, chemoreceptors (sensors that detect any change in oxygen, carbon dioxide and pH) are activated. Now what these chemoreceptors do is to in turn stimulate the sympathetic nervous system of the body (whenever you hear the word sympathetic nervous system, always remember that is associated with activities that will also increase efficiency of the body system).
The sympathetic nervous system tries to increase the oxygen level thus increasing the heart rate (tachycardia). Another thing the sympathetic nervous system does is to increase the rate of respiration (tachypnea). Wao, isn't that amazing? The increased heart rate obviously will try to ensure that enough oxygenated blood goes to the brain and other organs that need it.
Inflammatory cytokines in blood, what happens
Perhaps these inflammatory cytokines get into the blood, what happens? If you can recall what they did to the endothelial vessels in the lungs, that's exactly what they will do to blood vessels around the body's circulatory system.
They cause septic shock and at the same time cause blood vessels to dilate leading to capillary permeability or perfusions (I.e fluids leaking out of the blood vessels into tissue spaces). The resultant effect of this, is a drop in the peripheral resistant of the blood system, drop in blood volume, drop in blood tension and finally a drop in blood pressure.
The drop in blood pressure will mean that vital organs won't be able to get enough blood because there must be a minimal pressure required to push this blood into the organs. The patient as a result of this becomes hypotensive and when this happens, it leads to organ failure.
At any point vital excretory organs like the kidney and liver don't get enough perfusion of blood, they will be unable to effectively carry out their excretory function. Obviously in the kidney, you would expect an increased creatinine (a waste product from muscle metabolism), increase in blood urea nitrogen as an evidence of kidney damage.
In the liver, you obviously would expect an increase in the level of Alanine Amino transaminase (ALT) and Aspartate Amino transaminase (AST) which are the major biomarkers of liver damage. You could also have an investigation in the level of bilirubin and acute phase proteins such as C-reactive proteins, fibrinogens etc.
You can now see that the general activity that occurs are sequential. One leading to the other.
The incubation period
You might want to ask again, so when does one know when one is infected. The incubation period of this virus is eithin the range of 4-14 days or 24 days but basically 4-14days. (Incubation period of any disease is the time range from when you were infected to the time it takes for you to develop the symptoms).
Now you see why you are asked to atleast isolate yourself for atleast two weeks.
The reason why the patient coughs or sneezes (medically called sternutation) is because the lung or the nasal cavity is irritated by unwanted substances. Sneezing is a mechanism employed by the body system and it involves the lungs, muscles, bones and nervous system.
They are activated when the epithelial lining of the nose is irritated. Now that sporadic and involuntary explosion of air through the mouth/nose is what helps to clean and clear out the nasal (nose) cavity of whatever that is irritating it. In the case of this corona virus pandemic, they irritate the nasal cavity and the lungs.
Coughing on the other hand is also a mechanism used to clear the nasal cavity but precisely the lungs and the bronchial tubes of foreign substances and irritants. Some coughs are normal because they are needed to clear foreign bodies or irritant but in a situation where the cough becomes persistent and continuous (chronic), then it msans a very serious problem.
Corona virus victims cough continuously because of the damage the viral particles does to the lungs. Once an infected person coughs (travels as fast as 50mph and expels about 3000 respiratory at once) or sneezes (100mph and expels about 100,000 droplets).
The resultant force leads to the deposition of the viral respiratory droplets (in this case of corona virus) on nearby surfaces. You get infected by touching surfaces that have obviously been contaminated by the deposits of the viral particles. Hence the need for you to wear masks to prevent spreading or being infected.
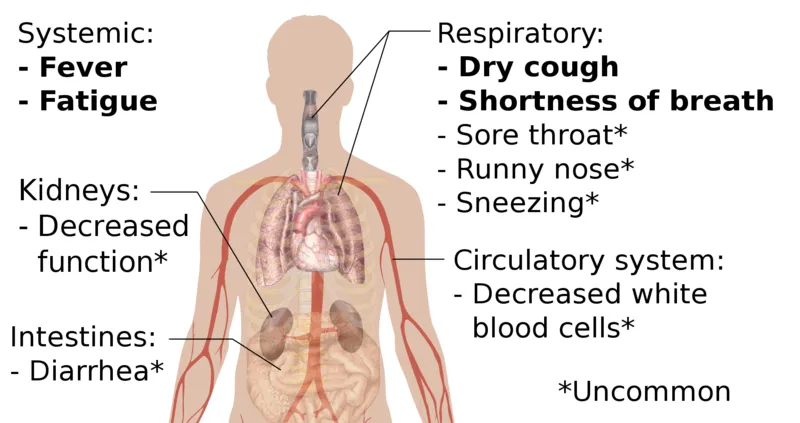
Usually patients with severe infection come down with fever (temperature above or equal to 100.4 degree F), severe and continuous cough dry cough and also shortnes or difficulty in breathing.
As of now, the gold standard for detection of this virus is the use of real time polymerase chain reaction (RT-PCR). To be sure and rule out that the patient is not suffering from a similar respiratory virus like influenza A or B, you must first carry out nasal pharyngeal swab using a swab stick.
You use swab stick to collect some amount of nasal swab for diagnosis. Once the influenza A and B have been ruled out, then you can now proceed to carry out what is referred to as the gold standard mentioned above.
Though this particular test takes a whole lot of time to be carried out in the laboratory and what you are trying to detect is the Covid-19 viral antigen. The samples for this test can be gotten from the blood, sputum of the patient and even from an aspirate.
A more complex test is the Nucleic Acid Amplification test, though this is far more expensive but it is much more sensitive then real time PCR.
Test like liver function test (you would expect an increased AST, ALT and Bilirubin), complete blood count (usually there is decreased white blood cells especially lymphocytes - lymphopenia).
In the kidney, you would also expect increased level of blood urea nitrogen and creatinine since the kidney is not perfusing well). There is an expected elevation in inflammatory markers like CRP, ESR, IL-6, increased lactate dehydrogenase (a general marker for most tissue damage though it is not specific for any particular tissue).
If the heart is not also perfused enough, you expect an increased level of treponin and CK-MB ( A specific biomarker of the heart injury). The last is the use of radiological technique, where you carry out chest X-ray, CT scan and finally Ultrasound.
The use of rapid diagnostics kits
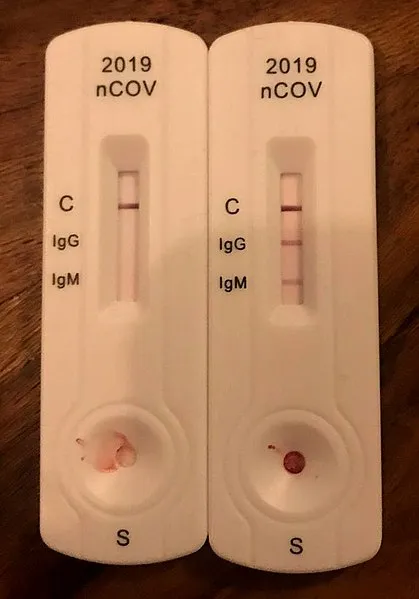
The infection of the body with any foreign agent (antigen) cause the body to produce a type of glycoprotein known as antibody. When the Covid-19 viral antigen gets into the body system, because it is foreign and not recognized by the body system, the body in turn produces antibodies against the virus.
Due to the complex processes and delay in time associated with the diagnostic methods above, using rapid diagnostic kits offer faster and quicker way to detect the presence of antibody produced against the viral antigen.
Principle behind the use of rapid diagnostics kits
In rapid diagnostic testing, the antibody produced against the Covid-19 virus is taken advantage of. It is expected that any person that is infected with COVID-19 will have basically two types of antibody - IgM and IgG antibodies circulating in their blood.
The IgM type are the first type of antibody to be produced against the virus and it simply tells us that the infection is recent while the IgG are developed later in the process of the infection.
The rapid diagnostics test strips is a lateral flow immunoassay technique and uses the principle of paper chromatography. It is a method for detecting the presence of an unknown analyte in a sample and this case - covid-19 viral antibodies.
The test strips are impregnated with conjugated antigens (antigens to which an enzymes substrate is attached to and produces visible colour change when it reacts with a corresponding antibody).
So when someone's blood that contains the viral antibody or antigen is collected and a drop is placed on the region where the enzyme substrate are impregnated, a complex is formed and by capillary action, this complex formed then moves along the test strip until it finds its corresponding antibody, binds and consequently produces visible colour change.
Subsequently after the complete part of this article, I will give a well detailed laboratory procedure on how rapid diagnostic test for most samples are carried out in the laboratory.
References
¶Video source under CC BY -SA ¶Covid-19 alert ¶Corona virus antibody detection ¶Wikipedia-corona virus pandemic ¶Science direct-corona virus ¶Hyperphysics- Laplace law ¶Chemoreceptors ¶WHO - advise for the public ¶Show your colours, only one way to wear surgical mask correctly with coloured side out ¶Sneeze vs cough ¶Disposable Surgical Face Masks: A Systematic Review ¶How to put on and remove a face mask ¶WHO- when an how to use the mask ¶Use of mask properly ¶Centre for disease control ¶WHO emergency diseases- Corona virus 2019 ¶World Health Organization- Corovirus ¶UNICEF- corona virus disease; what parents should know ¶Corona virus- symptoms, vaccines and risks ¶BBC- What misinformation has been spread in Africa ¶[WHO Laboratory testing for Corona virus in suspected human cases ¶Coronavirus disease COVID-19 technical guidance: Laboratory testing for 2019-nCoV in humans)
Return from Critical and detailed insights on COVID-19: All you need to know to cyprianj's Web3 Blog