The presence of cancer cells in the body circulation triggers the activation of T-cells whose job is simple; locate the cancer cells and destroy them. The unfortunate thing is that some cancer cells can circulate freely in the body without being noticed. You may want to ask, how are they able to do it? They are able to go undetected because some can attach to a receptor that is found on the human immune cells.
The binding makes them go hidden and they successfully avoid destruction by the immune cells. The PD-1 protein on immune cells is one protein that has been implicated and therapies that are targeted at blocking this protein help to unmask the cancer cells so that they can subsequently face the wrought of the immune system. We will look more closely into what protein gives the cancer cells this leverage as we go on.
In my previous article, I discussed a very interesting novel way through which cancer cells can be destroyed using a T-cell whose genetic configuration has been altered in the disfavor of cancer cells.
The treatment approach has been used and confirmed to be very effective against some types of cancers provided they have the CD-19 antigen on their surfaces to allow the effective binding of the CAR T-cells. For basic details about this treatment strategy, you can read the post here - Catching up with the Chimeric Antigen Receptor T-cell therapy for Cancer treatment: Cancer cure is no longer far.
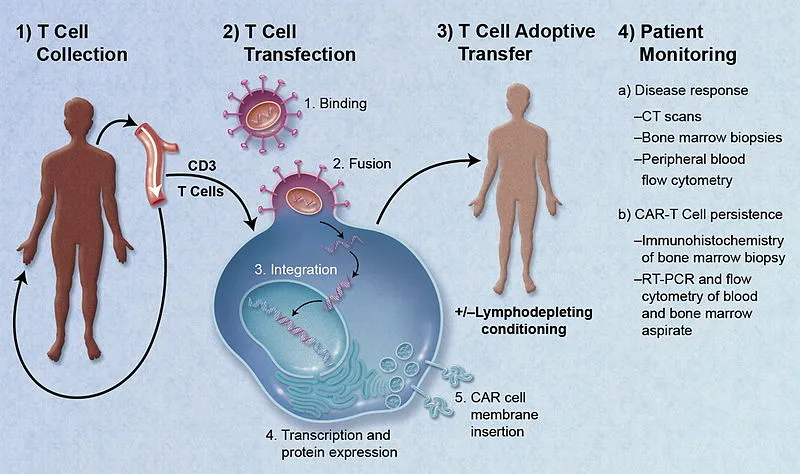 Adoptive cell therapy using CAR-modified T Cells
Adoptive cell therapy using CAR-modified T Cells
Today I intend to compare two very interesting procedures used in the management and treatment of cancer disease. The motivation to do this was through @lemouth's thoughts about my last post on CAR T-cells. Before I delve into the discussion properly, it will make more sense if I give a basic explanation to Keytruda, since we have already explained CAR T-cell therapy.
A basic understanding of keytruda will be of great help to us and at the same time, help us flow freely with the article. While explaining keytruda, the differences/similarities that exist between it and CAR T-cell therapy will also be elucidated. So sit tight and enjoy.
So what is keytruda all about?
Keytruda is also known as pembrolizumab is a type of immunotherapy and mainly employed in the treatment of cancer diseases. Keytruda is one of the many immunotherapies that employs the use of a special type of antibody in the detection and destruction of cancer cells. Even though it has a similar objective to the CAR T-cell therapy, and which is, the destruction of cancer cells, its mechanism of action is quite different.
Pembrolizumab is a full-length human immunoglobulin G4 (IgG4) monoclonal antibody directed against the immune checkpoint PD-1 to remove its binding with PD-L1 and thus restore an anti-tumor immune response of T cells. Pembrolizumab is one of the most advanced immune checkpoint inhibitors for cancer care.
Pembrolizumab works by targeting the protein called Programmed Cell Death Protein, PD-1 that is found on the human immune cells, e.g the lymphocytes. This is quite different from CAR T-cell therapy which targets the CD-19 located on the surface of the cancer cell itself.
In essence, it is obvious that both therapy work opposite ways but they still end up performing the job of cancer destruction. The big question here is, why does keytruda not target the cancer cells directly; why the human immune cells?
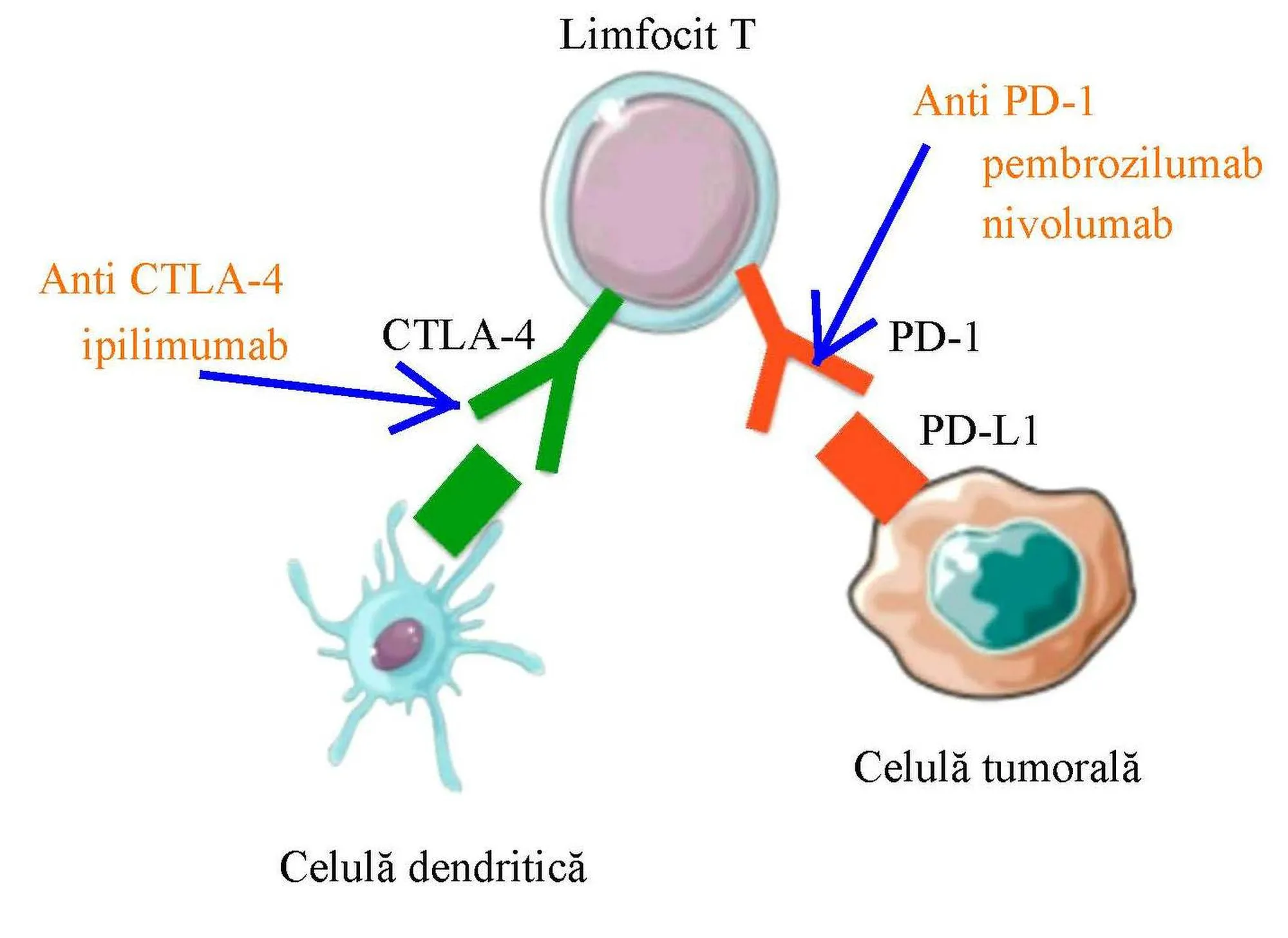 CTLA-4 and PD-1 monoclonal antibody
CTLA-4 and PD-1 monoclonal antibody
Though it targets the human immune system, it does this by indirectly stimulating it to fight cancer cells. Pembrolizumab operates similarly with Ipilimumab which targets the very molecule called Cytotoxic T-lymphocyte-associated protein 4, CTLA-4 aka Cluster of differentiation 152 (CD-152). Did you notice something about the names of the therapy, they both ended with -mab. we will discuss this in our next post, Let's deal with this for now.
The function of CTLA-4 in the body is to downregulate immune responses. This natural downregulation does not favor the body in the cased of cancer disease and preferably, it is better left not downregulated so as to enable the body to fight and destroy the cancer cells sufficiently enough to cause their remission (decrease in the signs of cancer effects). So the drug Ipilimumab acts by simply blocking the downregulatory function of the CTLA-4, thereby allowing the immune cells to fight the cancer cells.
The above is just how pembrolizumab operates but instead of the CTLA-4, the drug targets the PD-1 protein in the immune system. So what is the function of this PD-1 and why is it targeted? PD-1 is a regulatory protein in humans and mostly inhibits immune responses and promotes self-tolerance inside cancer cells. You find this protein more in T-cells that are highly specific for tumors or cancers, but since they have an inhibitory role on the T-cells, it makes it impossible for the T-cells to attack the cancer cells.
PD-1 is responsible for the provision of an attachment site for some cancer cells. The binding of cancer cells to this protein helps mask them from being detected by the cell's immune systems, most importantly, the T lymphocytes. The only way the cancer cells can be detected and destroyed is by blocking their attachment to the T lymphocytes.
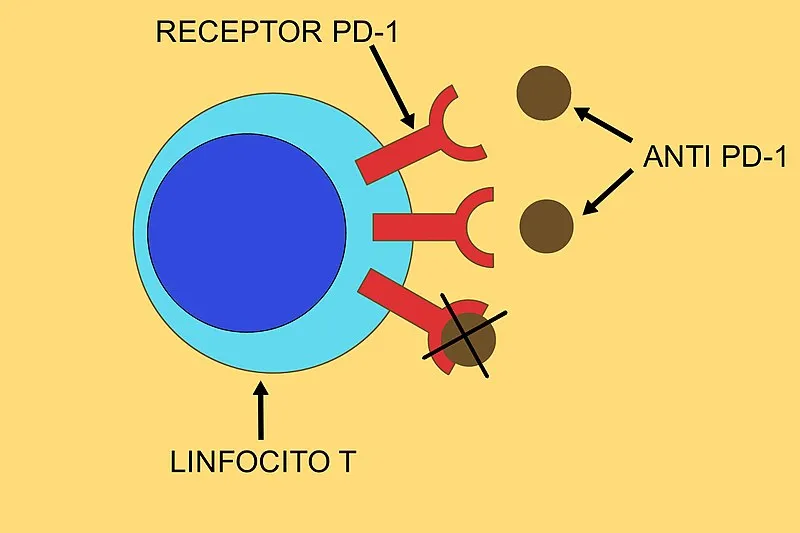 Pembrolizumab mechanism of action
Pembrolizumab mechanism of action
When this protein is inhibited, it helps the T-lymphocytes to be more effective by responding adequately against cancers. All these are achieved through the help of a monoclonal antibody which helps it in its specificity and binding to the PD-1 protein on the T-lymphocytes. For emphasis' sake, PD-1 is not only found on T-lymphocytes, you also find it on dendritic cells, macrophages, and of utmost importance, the natural killer cells.
As much as this PD-1 protein is hindering the destruction of cancer cells if not inhibited, they also have a natural role in the body. They mainly help differentiate between self cells from non-self cells and by so doing ensure that the immune cells do not attack their own tissues. If this is allowed to happen, it can cause autoimmune disease. One question you may ask here; How then are the immune cells able to detect cancer cells?
Cancer cells express antigens that are not of the human body's origin and as such, the immune cells are able to detect these antigens s foreign and immediately mount an immune response and attack the cancer cells. The problem is that cancer cells are faster in growth. Cancer cells grow faster than normal cells, since they are not regulated and not under influence of growth checkpoints.
From all we have said above, you can see that even keytruda indirectly kills the cancer cells by blocking the molecule preventing the immune cells from attacking the cancer cells unlike in the CAR T-cell therapy where the T-cells are equipped directly to attack and destroy the cancer cells.
Another similarity you would notice between both therapy is that they are both immunotherapeutic techniques since they both make use of the immune cells for the destruction of cancer cells. More specifically, Keytruda has been used successfully in the treatment of some types of lung cancer known as Non small cell lung cancer, cancer of the bladder, triple-negative cancer ( we will discuss this in my next post), Hodgkin lymphoma (the type of cancer that affects the lymphatic system) and even metastatic melanoma (another deadly and very difficult to treat cancer disease). You can read my previous article on CAR -T cell therapy to have a better understanding of what the lymphatic system is all about.
One of the benefits of the two therapies is that they both can be used to treat cancers that cannot be operated and secondly, they are very notorious for killing metastatic cancers (cancers with the ability to move and invade other normal healthy cells of the patient. While CAR T-cell requires the insertion of the chimeric gene insertion into the T lymphocytes, to enable it to identify and bind to cancer cells, pembrolizumab relies on a specific monoclonal antibodies for it to execute its function.
Further More, another important similarity between CAR T-cell therapy and pembrolizumab is that they are not necessarily drugs in the strict sense. In essence, they are not chemotherapy based. They do not directly attack the cancer cells but rather help the immune cells fight. But one of the likely limitations is that pembrolizumab while attacking cancer cells, could also attack normal cells, hence, the reason for serious side effects associated with it.
Secondly, treatment with pembrolizumab can cause an autoimmune reaction because the therapy knocks off the ability of the immune cells to correctly identify cells of their own. This ends up resulting in the immune cells attacking their own tissues and organs in some cases.
The most frequently cited pulmonary adverse effects of immunotherapy are interstitial lung disease and concomitant pneumonitis. Ipilimumab, a CTLA-4 inhibitor, has been shown to be a common agent responsible for pulmonary adverse effects
But hey! c'mon, who cares. I would rather prefer that the therapy kills the cancer cells and gives me chance of leaving for more years than allow the cancer cells shorten my life. The reward outweighs the risk.
Various reports have shown that both therapies work effectively in destroying cancer cells. In the United State for example, its approval has helped a lot of patients whose lives are already hanging on a balance.
Pembrolizumab has already proven its efficacy and thus obtained marketing authorization in so-called hot or hypermutated tumors or tumors expressing PD-L1 such as melanomas, non-small cell lung cancers, urothelial carcinomas, cervical cancer, etc.
Similarly with CAR T-cell therapy, these immuno therapy happens to be more effective than the conventional use of chemotherapies involving drugs like cisplastin
Since 2011, several large clinical trials of anti-CD19 CAR T-cell therapy have demonstrated excellent efficacy for patients with R/R B-ALL. With complete remission (CR) rates as high as 68% to 93%, it is now possible to offer a cure for some of these patients
The CAR T-cells are very powerful and they basically have some of the basic characteristics of activated T-cells. They can produce cytokines inflammatory proteins upon activation which causes cytokine release syndrome. These proteins are what help the cellular destruction of the cancer cells. One of the things that have been noticed in the patients is that those who have more than 50% of the cancer cells in their, body are more liable to suffer severe cytokine release syndrome while those with fewer leukemia cells suffer less or none at all.
Going further in a bid to solve this, it was discovered that another inflammatory protein called Interleukine-6 (IL-6) was responsible for the cytokine release. Since IL-6 is not required for T-cell activation. It makes sense to simply block it. Tocilizumab is the drug of choice to take care of this. It is quite interesting to know the science world is now one step ahead at every point.
I will conclude here by saying that, cancer is a disease that most times go unnoticed for a long and only begins to show its ugly face at a late hour, thereby leaving the patient at the mercy of death. Treatment with CAR T-cells and pembrolizumab aka keytruda works effectively on cancer patients and gives them more chances of survival.
As a side note; Breast and cervical cancer takes hits women more while prostate cancer hit men more.
As a woman, it is important to always do self examination and also go for cervical cancer screening to know the state of your cervical cells. As a man above 45 years, prostate test is very important. Increased prostate specific antigen (PSA), is a serious sign that should not be neglected. A permanent cure to the menace this disease causes, is of essence and that is why we will not rest until we win the war.
Until I come your way again, stay awesome!
References •Systemic adverse effects and toxicities associated with immunotherapy: A review •Keytruda (Pembrolizumab): First PD-1 Inhibitor Approved for Previously Treated Unresectable or Metastatic Melanoma •PD-1/PD-L1 pathway: current researches in cancer •Pembrolizumab •Clinical utility of pembrolizumab in the management of advanced solid tumors: an evidence-based review on the emerging new data •Efficacy and safety of anti-CD19 CAR T-cell therapy in 110 patients with B-cell acute lymphoblastic leukemia with high-risk features •CTLA-4: a moving target in immunotherapy •CTLA-4 and PD-1 Pathways: Similarities, Differences, and Implications of Their Inhibition •WHO recommends life-saving interleukin-6 receptor blockers for COVID-19 and urges producers to join efforts to rapidly increase access
Return from Evaluation of Keytruda and CAR T-cell therapy for cancer treatment: The similarities and differences therein to cyprianj's Web3 Blog