This post is the concluding part of this one - The aetiology and panacea of pain: exploring the orthodox and modern approaches to alleviation of pain in humans - 1 in which we critically discussed about pain, how they come about, transmitted through nervous system to the brain.
We also looked at the functions of the hypothalamus and the major role it plays in helping us understand pain and keep memory of it should there be a future occurrence. Furthermore, we looked at the reasons why animals have higher tolerance threshold for pain when compared to humans and more. To learn more, do visit by clicking the link above.
Our focus today will be to explain in clear terms how pain is inhibited through different means, and we will also look at what methods are available to do this. We will visit the medieval ways that have long existed before now and then we will then look at the various modern techniques. It sure will be an interesting read. Be rest assured you are in for a good deal. Join me as we tour through pain alleviation.
But first and foremost, let's fulfil our promise by giving an explanation as to why the brain is the only organ in the human body that doesn't feel pain. The reason is pretty simple if you read through our previous discussion on this subject. The human brain does not have pain receptors called nociceptors and as such, they cannot feel any form of pain. Nociceptors are scattered throughput the body and more in the skin but they are not found in the brain, and as such making the brain insensitive to pain.
The above is the reason surgeons can comfortably carryout surgeries on the brain without the patient feeling any form of pain. Infact, surgeries can be performed in the brain while the patient is fully awake. This however cannot be done on other parts or organs of the body. The patient must be given a sedative before the surgery is carried out.
So are there people that naturally do not feel pain?
The possibility of having people that do not feel pain practically exist. This occurs when people are born with a defect that results to an absence of nociceptors (pain receptors). Usually, this birth defect is mostly caused by gene abnormality. This could be as a result of mutation in the gene responsible for the expression and modulation of pain.
Mutations in the SCN9A gene cause congenital insensitivity to pain. The SCN9A gene provides instructions for making one part (the alpha subunit) of a sodium channel called NaV1.7. The SCN9A gene mutations that cause congenital insensitivity to pain result in the production of nonfunctional alpha subunits that cannot be incorporated into NaV1.7 channels. As a result, the channels cannot be formed. The absence of NaV1.7 channels impairs the transmission of pain signals from the site of injury to the brain, causing those affected to be insensitive to pain. Loss of this channel in olfactory sensory neurons likely impairs the transmission of smell-related signals to the brain, leading to anosmia.
This condition is usually congenital (birth defect prior birth) and affects the peripheral nervous system. In most cases, it has been reported to also be associated with anosmia (inability to sense or perceive smell). Notable cases of children born with this condition include the case of Isaac Brown, Ashlyn Blocker, report case of 4 children who were diagnosed of insensitivity to pain etc.
In as much as pain is undesirable, they still do have significant roles to play in our lives. Reports has shown that, majority of these individuals that are born with congenital insensitivity to pain do not live for long. They sustain severe injuries most often because they neither can differentiate nor know when a stimulus is compatible with life.
Congenital insensitivity to pain though rare, people are still born with it. Pain is the greatest teacher in life. Pain is the reason we avoid fire, venomous snakes, scorpion and mostly harmful substances or animals. One thing is certain, pain is our companion for life and we as humans have learnt how to deal with it. Lack of pain can be problematic for an individual.
Now we have a better understanding of this, let's now go further to talk about pain inhibition and how they happen in the body system. Are there natural physiologic mechanism set in place by the body to stop pain? If there are, how do they function. Do the effects of pain stimulus fade on their own accord, or are there already existing mechanism to neutralize pain? How were pain stopped in the mediaval times, with the use of drugs or other methods that does not involve the use of drugs. Is it possible for some people not to feel pain at all, if yes, how does it happen? Join me as we try to answer all this question.
All about pain inhibition
Pain inhibition is very important in some scenario as we have explained in the first part of our discussion on pain. Pain can be inhibited through several means; through natural physiologic means, through the use of drugs, through the use of certain procedures like the kinesiology, application of techniques in veritable energy medicine etc. You can read more about this type of medical approach here - The concept of energy medicine exploring the indispensable use of scintillating optic glass fibres in clinical diagnosis
Through natural means, the human body can inhibit pain, and it does this by releasing certain chemicals molecules that either block pain receptor sensitivity to pain stimuli or block the transmission of the pain signal to the brain. Either way, the ultimate goal is to stop pain. The beginning of every pain is inflammatory in nature no matter the etiology, so if the body can stop this inflammation, the pain will in the same vein stop.
One of the notable natural pain reliever of the body is the chemical known as endorphins. In another way, they are called collectively called Endogenous Morphines. Endogenous here means that they are naturally produced in the body while the morphine means it acts like opioids drugs. Endorphins are also referred to as wellness hormone because they are mostly released during stress.
Endorphins falls under the class of pain inhibitors called opioids and they mainly act by blocking the receptors involved in the neurotransmission of pain signal to the brain. They are released by action of the hypothalamus on the pituitary gland of the brain where they are stored. Their release does not only block pain but they also confer that sense of well-being in the individual, hence the reason they called well-being hormones.
Their concentration in the blood is seen to clinically increase significantly during prolonged stressful activities like exercises liking running, jumping, football etc. They help relieve stress and pain by their actions. This is why after strenuous exercise, taking some time to rest relieves you to some extent and over time, the body returns to normalcy due to the endomorphines released. Without these hormones, it would be very difficult for the to recover.
Through the use of artificially synthesized drugs, which could be opioids as well (they mimick morphine) or analgesics, pain is inhibited. One characteristic that is commonly seen in pain is inflammation. In pain, inflammatory cytokines are often released. While opioids like morphine, codeine, fentanyl, naloxone etc act on neurotransmission, others act on the inflammatory pathway associated with pain.
Drugs that act on the inflammatory pathway are referred to as Nonsteroidal anti-inflammatory drugs (NSAIDS). These set of drugs such as Diclofenac, ibuprofen etc. all work to inhibit the pro-inflammatory cytokines namely Interleukin 1 alpha (IL1a), Interleukin 1 beta (IL1b), Interleukin 6 (IL6) and Tumour necrosis factor alpha TNF-a). These cytokines are responsible for the various characteristics associated with the processes in inflammation.
These proinflammatory cytokines result in chemoattractant for neutrophils and help them to stick to the endothelial cells for migration. They also stimulate white cell phagocytosis and the production of inflammatory lipid prostaglandin E2 (PGE2). NSAIDs’ ability to interfere with the production of prostaglandin during the inflammatory cascade is the major mechanism cited for the anti-inflammatory success of these medications
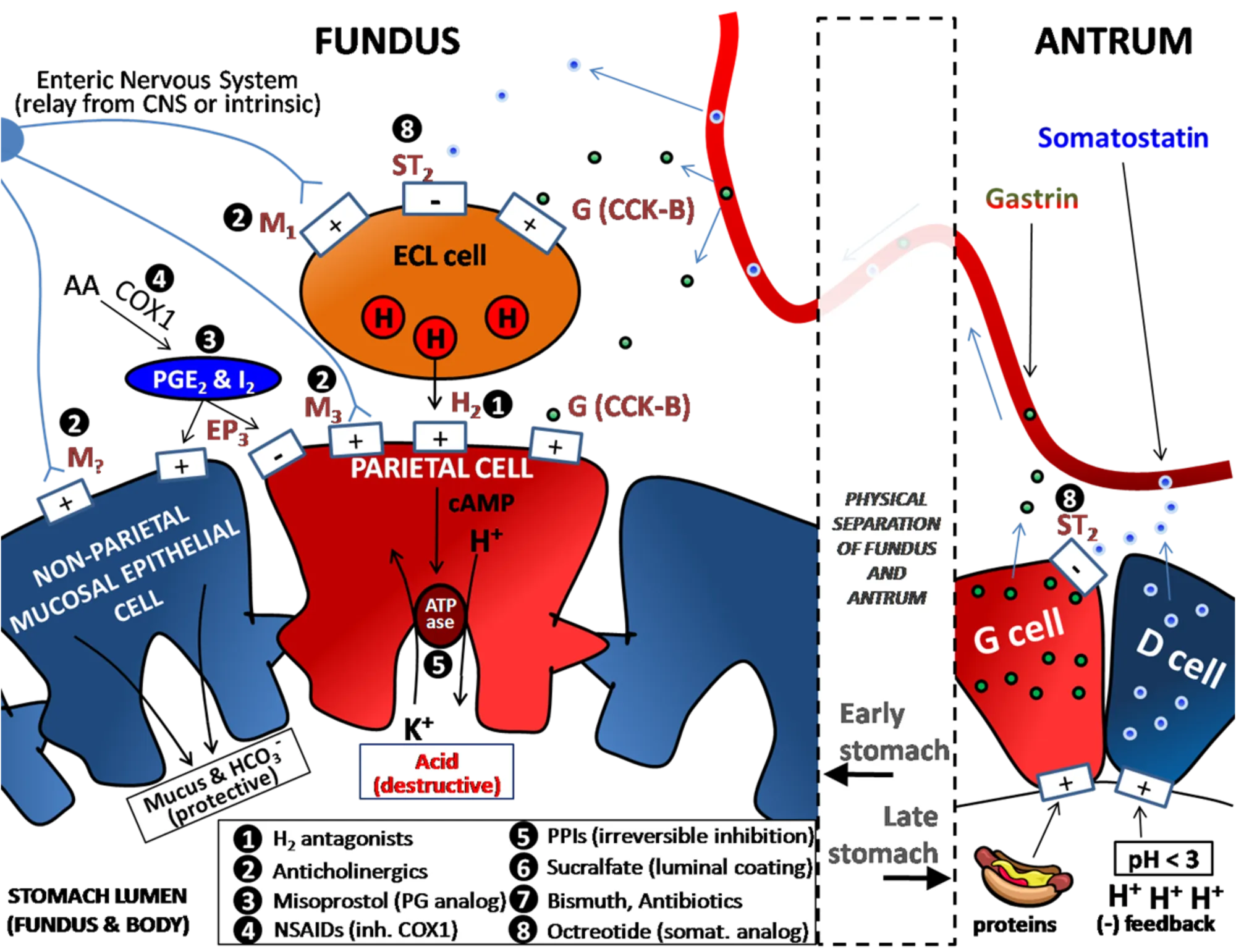 Inhibitory action of NSAIDs and how they contribute to ulcer formation in patients
Inhibitory action of NSAIDs and how they contribute to ulcer formation in patients
NSAIDs stop pain by simply blocking the major enzyme involved in inflammatory reactions that cause pain. The enzyme Cyclooxygenase-1 is responsible for the production of protective prostaglandins. In as much as pain inhibition is essential, it is not but without side effects. The inhibition of the protective prostaglandins which helps in the secretion of the mucous layer that protects the stomach epithelial lining from the destructive effects of the stomach gastric acids, puts the stomach at greater risk ol ulceration.
In essence, continuous use of NSAIDS can put the patient at greater risk of developing stomach ulcer since the mucous protective layer production has been inhibited by the drug. Not only do they block the secretion of protective mucous layer in the stomach, they also have negative effects on blood clotting in humans.
NSAIDs inhibit the production of Thromboxane A2 through their inhibitory action on the enzyme Cyclooxygenase-1. Thromboxane A2 helps in the formation of blot clots when we get injured or during bleeding. They help initiate platelet aggregation and clumping to stop bleeding. If these molecule is lacking, the tendency to bleed to death in any injury is sure inevitable.
While drugs like NSAIDs have their associated side effects, opioids similarly have theirs. They mostly create a state of dependency and addiction in the individual consuming them. Since they are act neurologically and are known for their creation of a state of well-being in the patient, they are the mostly abused. Aside the use of these drugs, there are other means through which pain can be alleviated and these procedures have to some extent proven to be effective. Let's take a look at some of them.
The principle of kinesiology
Some methods used in the alleviation of pains does not necessarily require the use of any form of drugs, rather some employ the manipulation of the body's muscles, tissues, joints and even tendons. The positions of these tissues can either have a positive or negative effect to pain initiation.
Wrong positioning of the hand muscle for a long time for example, can cause severe pain but when returned to its initial right position the pain subsides. This is taken advantage of in the practice of kinesiology. So what really is kinesiology?
Kinesiology is simply a study and practice that aims at improving motor functions in humans. By motor functions, we mean the musculoskeletal system that allows us move all parts of our body and even engage in physical activities.
Kinesiology is a diagnostic, therapeutic complementary therapy utilising subtle change in manual muscle testing results to evaluate the body's energetic balance and select healing modalities.
In addition, kinesiology aims to understand the basic principles underlying human mechanics and anatomy in relation to how we move and how pain resulting from our activities can be alleviated.
One of the notable and widely applied principle of kinesiology is seen in the use of Kinesio tapes. Some reports has shown that these tapes help relieve muscle pains and inflammation, improve muscular strength and movement and above all, they provide strength and support to injured muscle thus, facilitating easy movement.
While these treatment's approach remains highly debated with regards to its effectiveness, various reports have shown that it works despite some disbeliefs. Kinesiology is advantageous in the sense that it is therapeutic approach that is non invasive in nature and does not involve any complexity of any sort. This aligns with he ultimate goal in any therapy - treatment with less pain and maximum benefit.
Kinesio taping is commonly used on sport athletes with the intent of relieving them of muscle and joint pain, and at the same time, assist their muscle movement during injury. They play good role in ensuring that that muscle spasm does not occur in the patient.
Kinesiology tapes are flexible and highly elastic so as to enable them move freely as the muscles contract and relax. This approach to alleviate pain compares to veritable energy medicine that is also non invasive.
Conclusively, the use of opioids like morphine and heroin are part of the medieval means of alleviating pain in humans. Till date some of these drugs are still in use and the side effects they have is of great concern. With time, more unique ways to alleviate pain in patients without having to cause much side effects, will be the mainstay. Pain is a fundamental part of human existence whose absence can jeopardize our longevity in life.
References •A review of the literature in applied and specialised kinesiology •Congenital insensitivity to pain •Natural anti-inflammatory agents for pain relief •Opioids - mechanisms of action •Effects of nonsteroidal antiinflammatory drugs on platelet function and systemic hemostasis •Endorphins: The brain’s natural pain reliever •Chapter 8: Pain Modulation and Mechanisms •Congenital Insensitivity to Pain and Anhydrosis (CIPA) Syndrome; A Report of 4 Cases •Acute effect of kinesiology taping on muscle strength, tissue temperature, balance, and mobility in female patients with osteoarthritis of the knee •Kinesio Taping
Return from Exploring the orthodox and modern approaches to alleviation of pain in humans: how the use of Kinesio tapes have been beneficial - 2 to cyprianj's Web3 Blog