Welcome to the third episode of our workshop series where we use the microscope to unmask organisms that are hidden to our eyes. As usual, I wish to reveal those parasites and pathogens behind the aetiology of some disease conditions. I will continue to expose this microorganisms, how they infect and affect us as humans and the major negative roles they play in human health diseases pathology.
Without wasting much time, we will as usual start our discussion with an introduction to this protozoan and discuss in details all you need to know about them and how you can prevent infection by them.
Introduction
Trichomonas vaginalis is a parasitic protozoan (they are single celled and mostly infect larger animals). Being a protozoan, its major host is humans. Trichomonas are Pear-shaped in nature and they are highly motile. Interestingly, this parasite has a total of 5 flagella; 4 are located anterior while the remaining one runs through the entire body membrane and protrudes at the bottom. Their motility is facilitated by the flagella that protrudes from their end.
In men, they thrive in the prostate gland and the urethra orifice while in ladies, they are well abundant in the urogenital tract abd specifically the vagina hence, its name - T. vaginalis. They dwell in this region comfortably.
Infection with this parasite is mostly through sexual intercourse, so in order words, it is a sexually transmitted disease and has been reported to be mostly common in women. The disease caused by this parasite is known as Trichomoniasis. Surprisingly, the symptoms of infection with this parasite vary among individuals i.e you might be infected and won't know while another might be infected and begin to present symptoms of infection with the parasite.
In women, they usually experience green or yellowish smelly discharge that has fish odour. Some also will experience pain while urinating as well as severe burning sensation which is as a result of the inflammation visible as redness/soreness of the urogenitalia. Men also experience similar symptoms as women but with further burning sensation after they ejaculate (the climax of sexual intercourse in men, characterized by the forceful ejection of semen).
The life cycle of this parasite is quite simple and not complicated as seen in other parasite we have discussed. They really don't need any intermediate host. Infection is simply through sexual intercourse between a male and a female. Depending on who is infected, the parasite can migrate from the penis into the vagina and vice versa. This occurs mostly in people that have multiple sexual particular and also those that engage in sexual activities without any form of protection.
They damage the epithelial walls of the urogenitalia thereby causing inflammation. This consequently results to erosion of the epithelial walls. The side effects of this parasite is causes what is known as strawberry berry cervix in women. They make the cervix have small red like lessions that is caused by the internal slight bleeding.
Infection with T. Vaginalis increases the chances of infection with HIV because they expose the cells through the injury they cause to this virus and makes its entrance much more easier. Infection with T. vaginalis is very common.
Diagnosis
To diagnose this parasite is also very simple and the major thing looked out for is the presence of the trophozoites in sample collected. A type of sample called High vaginal swab (HVS) is collected in women using the swab stick. This is also similar in men.
To collect sample for HVS, the first thing done is to use a speculum to dilate the vagina orifice (in women). You then simply insert the swab stick into the vagina. By rotational movement, you gently rotate the swab stick on the vaginal epithelium while scrubbing it as well to get enough the specimen. After this, you then gently remove the swab stick and return it into its packing that serves as a preservative for the specimen collected. Some of this preservative could be Charcoal based.
The preservative keeps the microorganisms alive and active do that they could be studied effectively using the microscope. Usually, it is better to examine the sample as soon as possible once collected. This increases the chances of seeing the active and motile parasite live. The longer they remain in the preservative medium, the lesser the chances of seeing them move. Most will likely die off overtime.
The difference in sample collection is mainly in the type of swab used. In men, urethral swab is used. For specific diagnosis, you can go further to do a culture (grow the parasite in a media that encourages And enhances their growth) after which you then stain using any staining technique for coloured visualization of the parasite. Note at this point that, staining cannot help you observe the motile organisms rather, it only helps to give you an in-depth characterisation of the parasite.
Staining the parasite will help reveal those attributes of the parasite. It reveals the nucleus, flagella etc. Clearly for you to understand but for basic knowledge sake, we are more interested in having a basic idea of how this parasite look in an unstained specimen aka wet preparation (wet prep). Wet preparation is primarily for motility. It ensure that the parasites are free to move and thus enables the observer to see them as they move under the microscope.
For quick diagnosis, wet prep is always done and it is very simple. All You need is a grease free clean glass slide and normal saline. You first place a drop of normal saline on the glass slide and then using the swab stick containing the specimen, you make a smear by gently turning the swab stick in the normal saline on the glass slide.
Place a cover slip over the smear and then view under the microscope. Rotate the nose piece of the microscope to x10 for focusing and then you use x40 to view the smear. Preferably as earlier said above, view as soon as possible so as to increase your chances of seeing the live motile paray. If the parasite is present in the sample collected, you will see them move actively in wet preparation you made. This is the moment you have being waiting for, let's take a look at the images of our findings as usual.
Results and findings
The images below displays T. vaginalis under wet preparation using X40 objective lens of a light compound microscope.
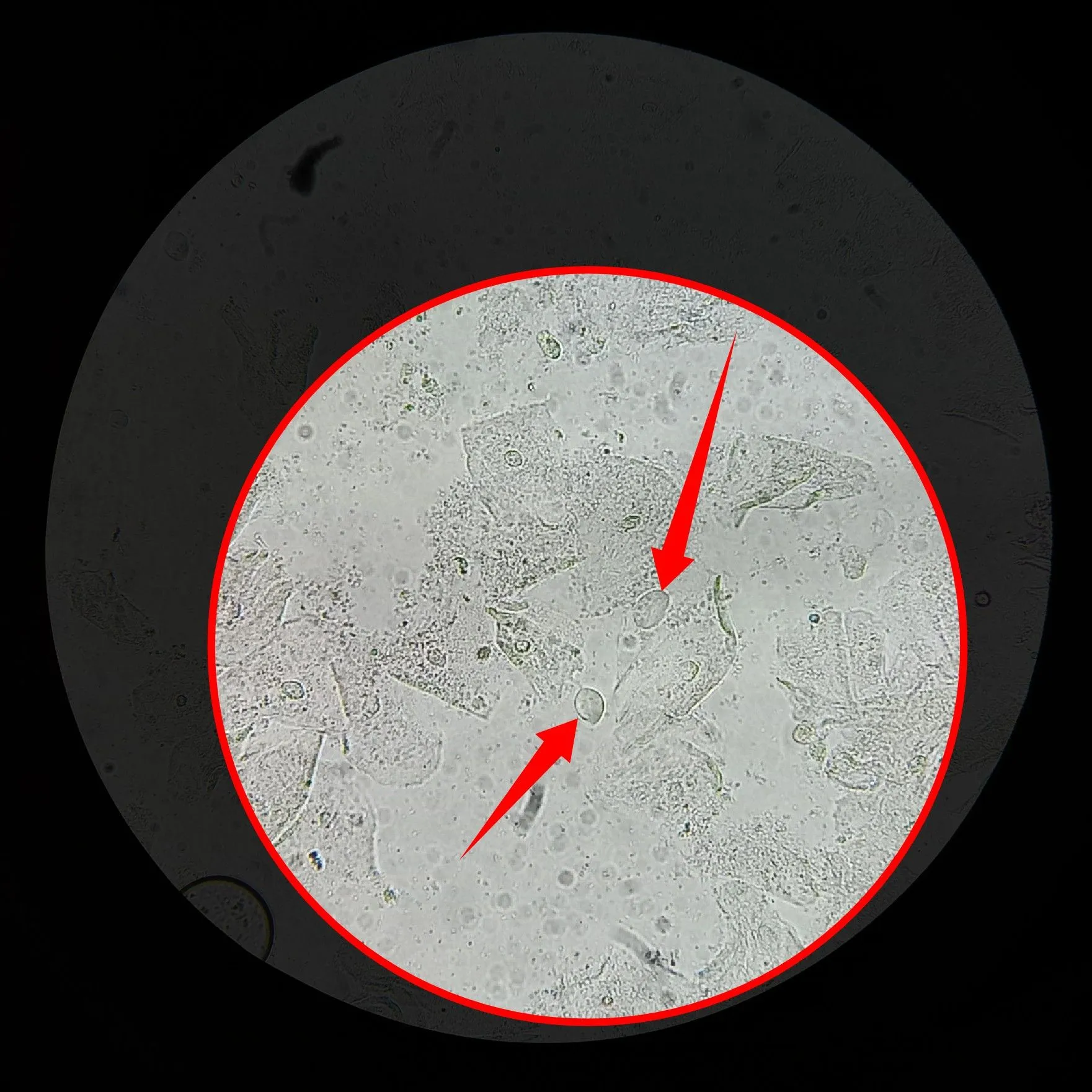
Observe the pointed structures in the image above and you would see that it has close resemblance with the images we have used earlier on while discussing the parasite.
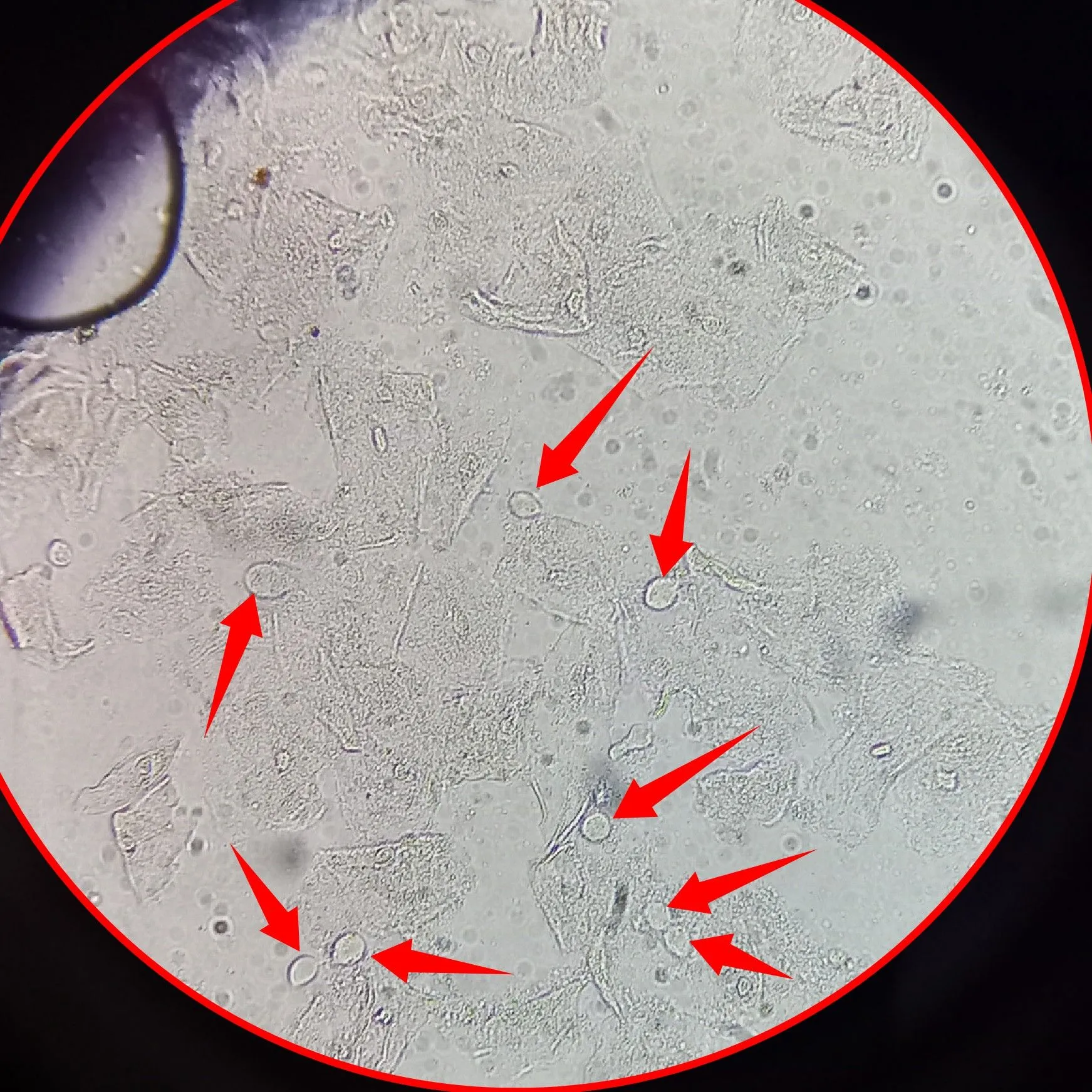
Usually, under wet preparation, you would not really expect to see all the features like the anterior flaggela and nucleus possessed by this protozoan, but one thing is certain, the flagella they used for movement located at the bottom are usually in most cases present. Secondly, you identify them also with their shape which is oval.
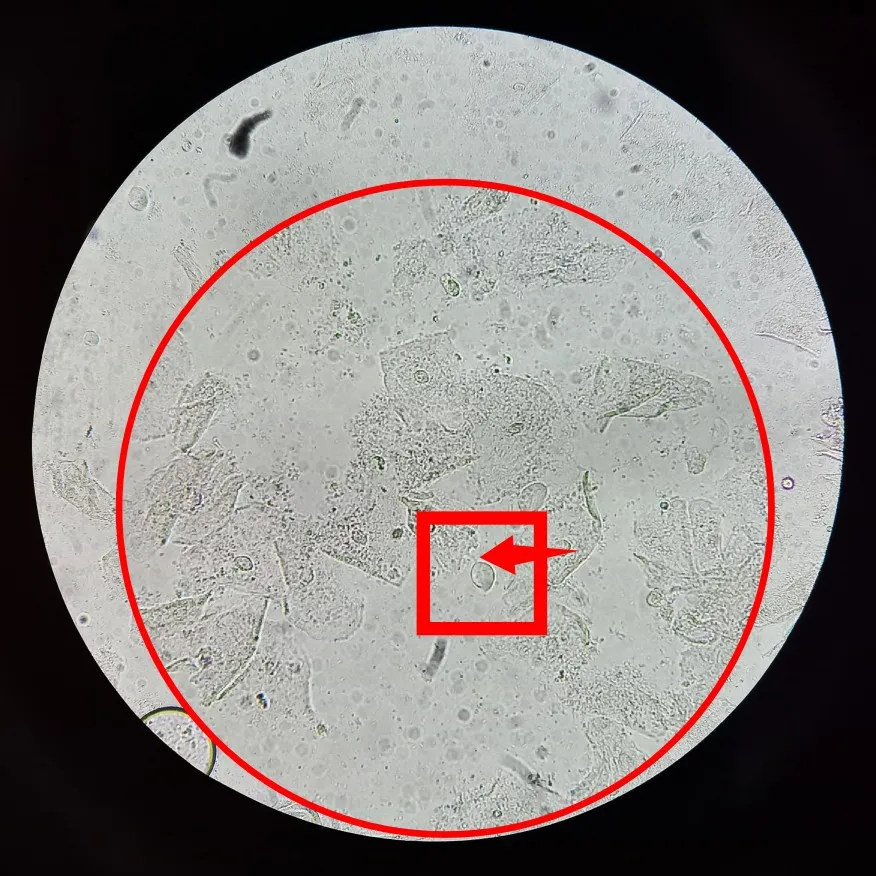
The image above points directly to the fifth flagellum of T. vaginalis mainly used for locomotion located at the bottom of the parasite. In some cases, the flagellum for movement might not be so visible, but you will still observe the random movement of the parasite under the microscope.
Be careful not to confuse the nucleus of epithelial cells to be trophozoites of T. vaginalis. This confusion usually sets in when the parasites are already dead either due to delay in making the wet preparation for microscopy of due the use of wrong media for their preservation.
The nucleus of epithelial cells that line the vaginal or urethral wall looks almost like the trophozoites of T. vaginalis and if you are not observant enough, you might think they are T. vaginalis. Remember we earlier explained that this epithelial cells lines the vaginal and urethra, and they mostly shed off in large amount during infection with this parasite.
In the process of sample collection, this epithelial cells are usually picked up together with the parasites, and by mere looking at a wet preparation under the microscope, you can easily tell the source of the specimen.
Epithelial cells are usually larger and flat in size with a darker small nuclei almost at their center. They are almost round in shape sometimes.
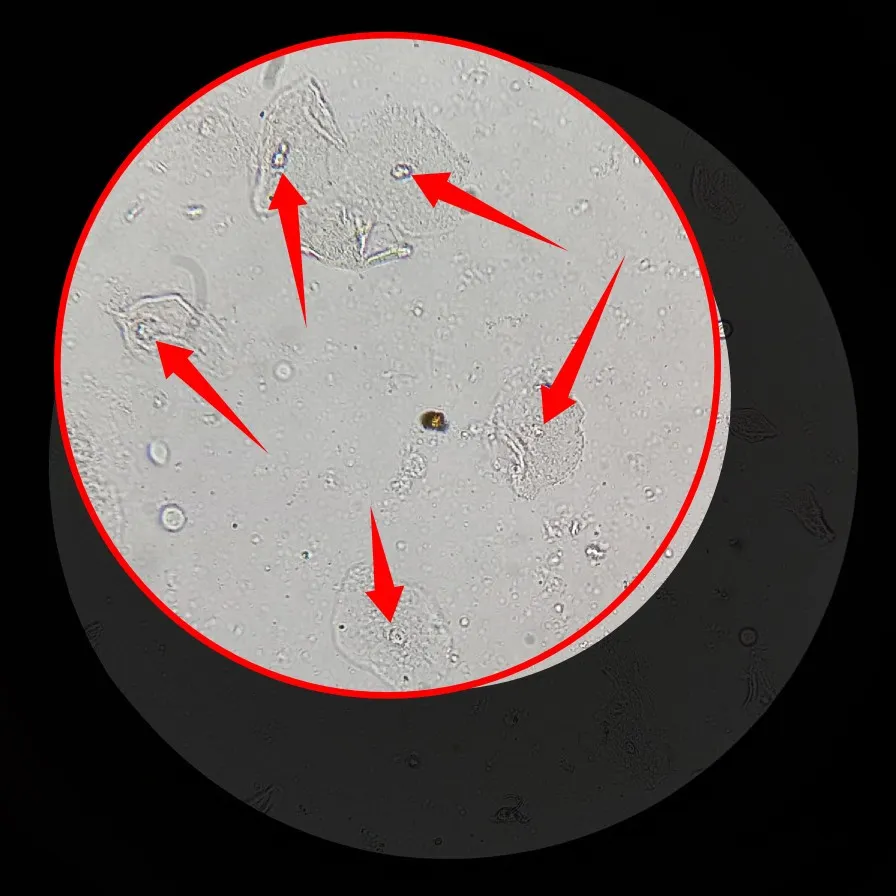
In most cases, T. vaginalis is slightly bigger than the nucleus of the epithelial cells. But all things being equal, the hall mark for easy identification of this parasite is their movement in wet preparation. Going further to stain the parasite only but double confirms its identity. I sure did a a video of the parasite for your viewing pleasure, enjoy.
Please don't mind the noise in background. Some days are like that. Trust you observed the actively moving trophozoites. A colleague of mine calls them, the dancing bubbles, haha.
Clinical significance and treatment
The presence of this parasite in the specimen is a clear indication of Trichomoniasis, the disease caused by this parasite. Treatment of this also easy and infact, it is one of the most treatable sexual transmitted infection. Administration of Metronidazole is the drug of choice for the treatment of trichomoniasis.
Conclusion
As much as the infection is easily treatable, it is still better to avoid unprotected sexual intercourse with multiple sex partners. The disease increases one's chances of contracting HIV. If you must engage in sexual activities, please use protection for your safety and that of your partner.
Until I come your way, stay safe!
References •Methods for Detection of Trichomonas vaginalis in the Male Partners of Infected Women: Implications for Control of Trichomoniasis •Clinical and Microbiological Aspects of Trichomonas vaginalis •Trichomoniasis
Return from Medical laboratory workshop Episode 3: (Live view of motile Trichomonas vaginalis trophozoites) to cyprianj's Web3 Blog