This article is a continuation of my last discussion on pharmacokinetics of drugs. I implore you to read the previous article if you haven't, doing so will bring up to speed on what I am about to write on.
Like I previously explained, the elimination of a drug by product is very important otherwise, it will cause a serious health problem if they are allowed to accumulate in the body system or probably when the clearance mechanism or organs fail to perform this duty. The liver and the kidney and the lungs are the three major organs responsible for drug clearance. So before we go deep, let's define what drug clearance and the kinetics of drug clearance really means.
Like I would always do, give you the simplest definition. Drug clearance or elimination simply means the volume of plasma in the the body system or vascular system that is cleared of a drug a particular drug per unit time through the process of metabolic and excretion. The word kinetic simply means motion or movement, so in relation to drugs, it means the movement of drugs.
Now it is very important I emphasise on this, the clearance here is not referring to those drugs that are bound to plasma protein rather, it is referring to the drugs that are free and unbound in the blood. Drugs that are bound to plasma protein are usually active and still exerting their therapeutic effect and as such are not available for metabolism. Hope you understand? Alright, let's continue!
The clearance of a drug is likened to the concentration or the amount drug left in the systemic blood circulation after the drug administration. Basically, the elimination of clearance of a drug occurs by the perfusion (entrance) of blood to the various organs that are involved in the removal or extraction of the drug from the blood system. Remember we said in the previous article that, organs that receive much cardiac blood output play crucial role in the drug distribution.
What the above invariably means is that, organs that receive a greater percentage of cardiac output will be much more involved in the drug clearance. This is very obvious because the liver, lungs and the kidney receive greater percentage of blood from the heart than other organs, and as such are the major organs involved in drug clearance and excretion.
The order kinetics
The excretion of a drug could either follow a first order or zero order kinetics. Don't worry, I win explain this. Remember, the amount concentration of a drug in the plasma is related to the volume of distribution, Vd thus, we can easily get the elimination rate constant, Kel by using the expression below:
Kel = Cl/Vd
First order kinetic:
This is also referred to as a linear process and it simply means that the rate of the drug excretion moves at a rate that is dependent on the concentration of the drug in the body system. The higher the concentration of the drug, the faster they are eliminatied. 95% of the drugs we take follow the first order kinetic for elimination. If the process is not linear or does not follow the first order kinetic, the elimination process will be saturated and will ultimately lead to accumulation of the drugs in body. Hope you now see the importance of studying the kinetics of its drugs.
Zero order kinetic:
This is a non linear process. In zero order kinetics reaction is constant and moves at a rate that is independent of the concentration of the drug in the body. What it means here is that, regardless of the concentration of the dug in the body, the elimination process of the drug is always saturated. Drugs like phenytoin, cisplastin, omeprazol etc are always eliminated through the zero order kinetic.
The major key players in total clearance - liver and kidneys
The total clearance, Tcl of a drug is simply expressed by the equation:
Tcl = ClH + ClR + ClL Where ClH, is the hepatic clearance, ClR the renal clearance, and ClL lung clearance.
Hepatic clearance and renal excretion are mostly involved in the extraction of drugs from the body while the lung is involved in the excretion of gaseos substances. Succinctly, we will pick each one after the other.
Hepatic (liver) or biliary clearance
Hepatic clearance is the clearance of a drug is the rate of the drug removal divided by its plasma concentration in the vascular system - artery. The detoxification and clearance of drugs is championed by the liver via glucuronidation and then subsequently excreted into the bile, thus the name biliary excretion. It is able to do this because it houses the major enzymes that are involved in drug metabolism.
The liver as an organ secrets about 0.25 to 1liter of bile everyday. Drugs and their metabolites are excreted by the liver into the bile which is stored in the gall bladder, the gall bladder further empties its content into the intestine and in the process, the metabolites are excreted out of the body in faeces.
It contains mixed function monooxygenase enzymes. A well known one is the Cytochrome p450 enzyme. In the liver, drugs cleared are those that have been either metabolised or those that are unabsorbed. After the detoxification of the drug by the hepatic system, they are excreted through faeces from the body.
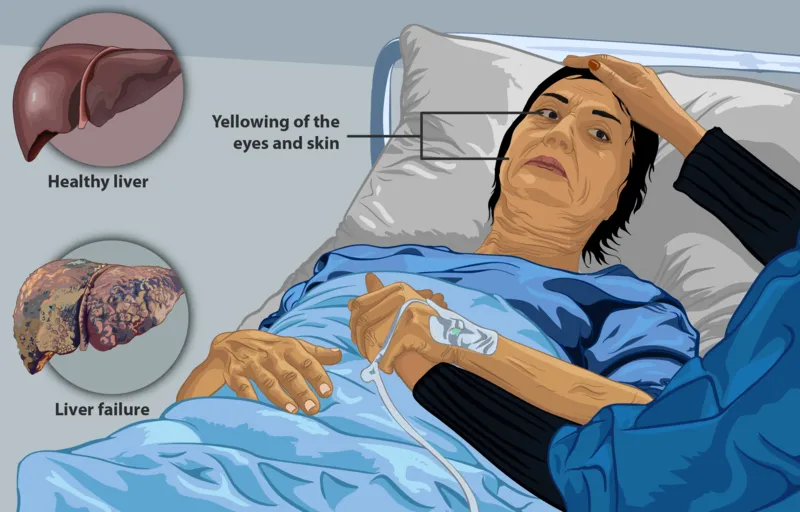
The liver is saddled with a great deal of responsibility of detoxification. Due to its high regenerative ability, a damage section a liver can repair itself unless the damage continues indefinitely. This is why most times people with liver disease some times never notice that there is a problem until it has reached a critical stage. But with early diagnosis and detection treatment will go a long way. The major signs of liver problem is yellowing of the eyes and the skin (jaundice). This occurs due to the increased concentration of bilirubin in the body.
Treatment of jaundiced infants
Some kids are born jaundiced due to haemolytic anaemia of the new born - a condition that causes the destruction of the red blood cells which results to the release of bilirubin (a bile pigment) from the red blood cell. The continual destruction of red blood cells causes the level of the bilirubin to be very high in the infants body leading to its accumulation in the eyes (eyes become yellow coloured), skin and brain and ultimately causes a disease condition known as kernicterus.
Bilirubin is able to cross the blood brain barrier and when they accumulate too much in the brain, they cause a could cause serious brain damage - athetoid cerebral palsy and even hearing loss.
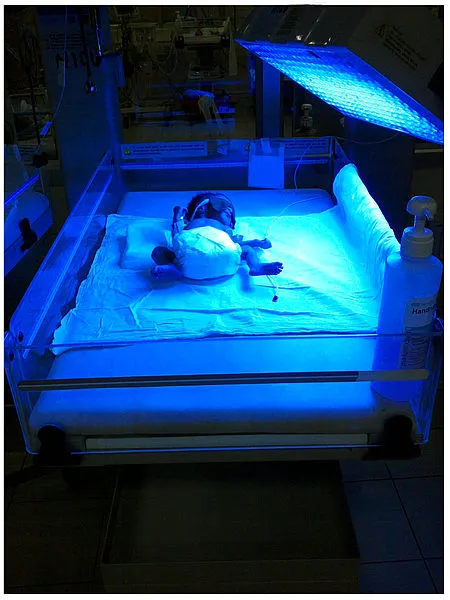
If you have ever had the opportunity of being in a paediatric ward in the hospital, you would observe some babies are kept inside a chamber under a light bulb illuminating them, there is a reason for that and you will find out why soon. Take a chill pill and relax, it's quite interesting, trust me.
Going the traditional way
Traditionally in the past, when children have jaundice, they are exposed to filtered sunlight under a canopy to treat jaundice. Imagine the stress and pain the mother and the child have to go through just to get rid of bilirubin.
The principle behind this is that, sunlight ray or heat breaks down bilirubin to a water soluble and less toxic form known as biliverdin that subsequently dissolves and it's eliminated from the body.
The introduction of advanced phototherapy
Technological advancement resulted to the development of a more advanced technique of using phototherapy to treat neonatal jaundice. Here the baby is kept in a chamber as well but this time around, under a blue/white light. The light radiation helps to breakdown bilirubin and converts it to beliverdin just as I earlier explain.
The benefit this offers is that, the mother need not keep the baby under the heat of the canopy as this causes stress and unnecessary discomfort to both the mother and the child. Though this method still has some flops and one of which is, a possible damage to the baby's eyes by the led light. Further technological advancements have produced a more convenient phototherapy tool called the Biliblanket.
A further step ahead - the Biliblanket
Due to the shortcomings associated with the use of the led phototherapy technique, a more easy, portable and very convenient device has been produced which can also be used to treat neonatal jaundice. It is referred to as a Biliblanket. It is so called because of its nature and portability. One of the beautiful thing about this device is that, home therapy can be performed using it thus saving the mother or family inpatient treatment cost in the hospital.
How this novel Biliblankets device works
The biliblanket is made of a pad of wooven flexible optical fibres that produce blue/white lights of changing intensities that permeate through a light fabric. For the treatment, the baby is placed on the blanket and then the biliblanket is tied to the back of the baby. Once this is done and the light is turned on, they will help breakdown the excess bilirubin that causes discolouration of the skin and eyes in the baby.
Biliblankets offers greater advantage over the older methods because the mother doesn't need to worry about keeping the baby lieing inside a chamber with led lights. In the course of treatment, the baby can be held, clothed, nursed and generally taken care of by the mother. It does not need the baby to be separated from the mother, neither will the baby be allowed to lie alone in the box with their eyes covered.
With this setting, the mother can easily breaat feed her baby while treatment is on going. The technology focuses more on body or back of the baby and not the face, hence no need to cover the baby's eye. Also, the light is more concentrated on the baby that the other methods in which lights are dispersed. Finally, the portability of the device is just awesome. Clearance of bilirubin just got much more easier and less complicated with the use of biliblankets. Lets round up our discussion on clearance kinetics with renal clearance.
Renal clearance
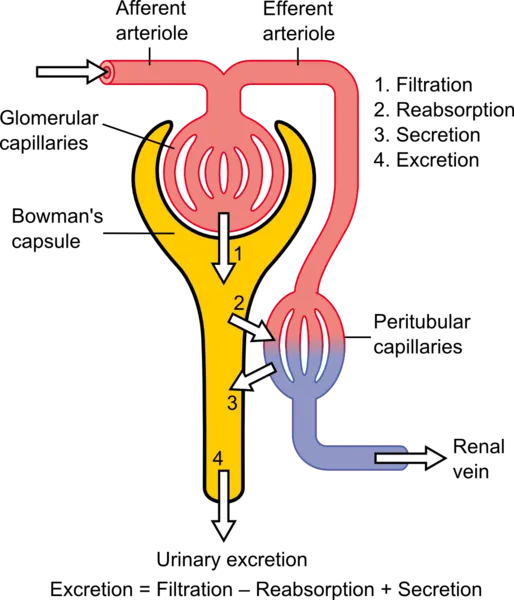
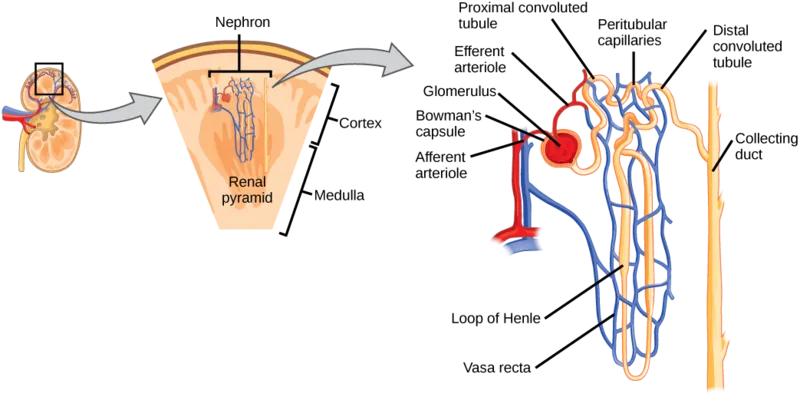
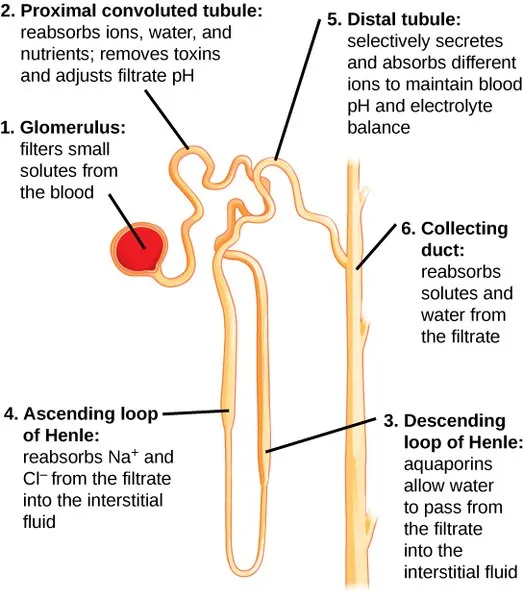
The renal clearance of the kidney is mostly made up of liquids in which solutes are dissolved in. This majorly reflects the excretion of drugs into the urine by the organ - kidney. The functional unit of the kidney that is fully involved in the excretion of drug is the nephron. Let'a quickly see how this is done.
The nephron is made up glomerular capillaries (bunch of packed tiny blood vessels), which is mainly responsible for the ultrafiltration of blood that is supplied to the kidney by the afferent arteriole. The glomerullar capillaries are held by the bowman capsule which extends into the lumen of the nephron and also plays crucial role in the filtration of blood. When blood enters the kidney, three things happen before excretion of the drug through the urine.
First of all, filtration must occur in the bowman capsule and this is done by the glomerulous. So here, the drug or it's metabolite is filtered out of the blood into the lumen. A damage or inflamation of the glomerulous leads to a condition referred to as glomerular nephritis and it results to blood being present in the urine. After filtration what happens next is reabsorption of fluids and electrolytes in the proximal tubule, loop of henle, and the distal tubule.
Reabsorption is essential for homeostasis and electrolyte balance in the body system and it mostly occurs in the ascending loop of henle. Reabsorption also play a role in the nature of the urine - acidic or alkaline urine. During reabsorption in the proximal convulated tubule, water, ions and nutrients are taken up while drug metabolites and toxins are not.
After reabsorption, the next is Secretions. Secretions occurs simultaneously with absorption. What this means is that, it is not a must that one must occur before the other rather, they work hand in hand. Secretions occur mostly in the distal convulated tubule. Here selective secretions and absorption occurs and this area ensure that the blood pH and electrolyte (Na, K+, Cl-, HCO3-) concentration are in balance.
Always remember this, the acidity or alkalinity of a urine lies on the selective secretions and absorption that occurs in the distal convulated tubule and the collecting duct most times. Finally, the filtrate is moved to the collecting duct where further reabsorprion of solutes and water from it occurs. This area of the kidney also concentrates the urine produced and it is at this point you get to see high concentration of the drug metabolites or its unchanged form if any.
When excretion becomes problematic
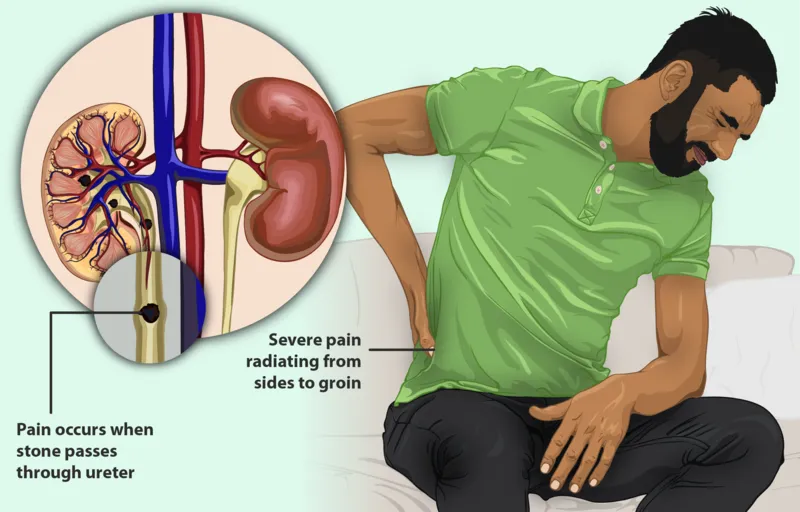
Problem could ensue when the urinary pathway from the kidney is blocked by kidney stones - excess mineral filtrates that have accumulated over time, the most common one is the calcium stone, usually made up of both calcium and oxalate (oxalate, a very common natural chemical that is found in most food we consume), calcium phosphate, struvite stones (formed when you have a type urinary tract infection that allows a bacteria to produce ammonia that over time accumulate in the kidney) and Urate crystals from uric acid.
How kidney stones are formed
Kidney stones are generally formed as a result of the continuous build up of dissolved minerals like magnesium, calcium, phosphate etc in the kidney, most especially the inner lining of the kidney. The major cause of kidney stone is lack of adequate water intake. It occurs most time in peopple that don't take in enough water to dissolve or dilute this minerals adequately.
Take the uric acid for example, which is usually formed when the urine is too acidic due to inadequate water to dilute it. Uric acid can either be formed alone or in combination with calcium when urine is too acidic. So always bear in mind, when you don't take in enough water, the urine becomes too acidic, the resultant effect is the formation of kidney stones. Hence, the need for us to be adequately hydrated all the time.
Did you know that most tablets drugs contain calcium phosphate
Bear this in mind, some of the tablet drugs we take contains calcium which act as a binder. It helps holds other constituent of a drug together. Especially drugs produced as tablets. This is one subtle way calcium also builds up in the system. So do ensure you take enough water to dilute this excess mineral
Little experiment to confirm if it is present
Get a glass of water and drop a drug tablet inside, if it contains calcium, after sometime, you would observe some whitish particles floating on the water, 90% those are calcium.
In conclusion, stay hydrated all the time, prevention is always better than cure!
Stay healthy.
References
•filtered sunlight a safe low tech treatment for new born jaundice •what is biliblanket therapy •Pharmacology - Elimination kinetics •BiliBlanket phototherapy system versus conventional phototherapy: a randomized controlled trial in preterm infants •what Biliblanket phototherapy is all about •Kidney stone causes, treatment and symtoms •Kidney stones types and their various compositions •Everything you need to know about jaundice •The nephron basic structure and function •Biopharmaceutics and pharmacokinetics •Clearance of drugs •Introduction to drug clearance •Calcium Phosphate in Pharmaceutical Product Development
Return from The kinetics of drug elimination/clearance to cyprianj's Web3 Blog