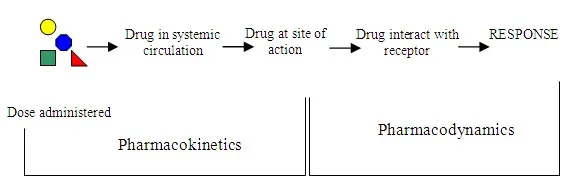
From our main last discussion on the pharmacokinetics of drugs, we where able to understand that pharmacokinetics means, the processes involved in a drug's absorption, distribution, metabolism and the excretion of its toxic or non toxic metabolites from the systemic circulation.
We were able to understand that pharmacokinetics simply means how the body handles a drug. Today, we will succinctly discuss the about Pharmacodynamics and it's associated terminologies. Let's do this , shall we!
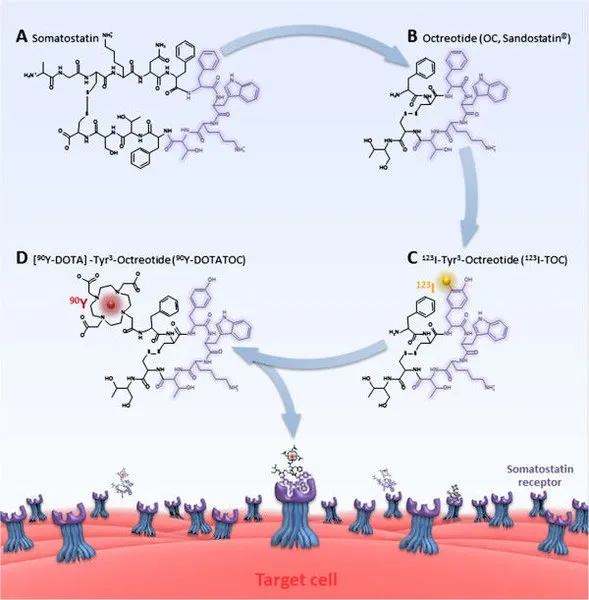
We will briefly discuss about some concepts that are indispensable before going into the real deal about pharmacodynamics. Just to remind and bring you up to speed, the general mechanism of drug actions is their binding to biological targets. Their binding leads to conformational change in the receptors which in turn leads to a biological response.
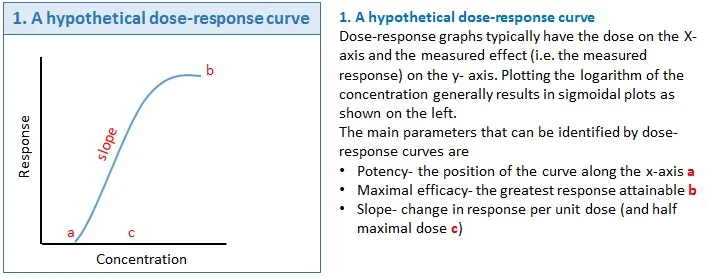
The action of the drug could either be full or partial and this brings us to the two very concept in Pharmacodynamics - Emax and EC50. The concept of Emax, this is the maximal effect a drug can produce on any parameter that is being measured. Another one is EC50, which is the concentration of the drug which produces half of the maximum effects at a very steady state.
Pharmacodynamics is the near opposite of pharmacokinetics as it relates to how drugs we ingest affect our biological system. Pharmacodynamics is simply the study of the physiological, mololecular and biochemical effects of a pharmaceutical drug on the body. The concept of Pharmacodynamics places major emphasis on the dose-response relationship.
To further clarify the above, Pharmacodynamics is all about the relationship that exists between a drug's concentration and its effects on the site of action. Drugs generally bind to receptors before they exert either their physiologic, biochemical or pharmaceutical actions. You cannot talk about drug actions without full understanding of the concept of drug-receptor interactions. Pharmacodynamics is anchored on three main points and they include:
•Receptor binding and sensitivity •Post receptors effects and •The chemical interactions of the drugs.
The three above are the main focal point on which Pharmacodynamics of drugs stands on. We will pick each point and elaborate more on them for a better understanding of the concept of Pharmacodynamics. You are sure to learn a lot here. Let's begin with the first point.
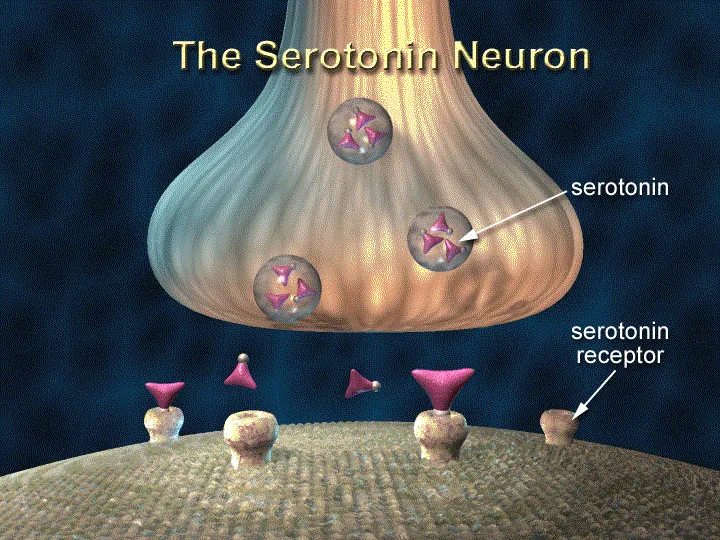
Receptors are glycoproteins that are located in the cell membranes of biological tissues. They could be intracellular (within the cell membrane) or extracellular (outside the membrane). Those that are found outside the membrane of the cell sometimes transverse across the membrane into the cell. They recognize ligands (drugs) and bind to them. Just like I pointed out earlier, drugs bind to receptors in order to exert theirs pharmaceutical actions.
Now the pharmacological response as a result of the binding in turn depends on whether the drug binds to its target or not. In the same vein, the drug's effects effects after successfully binding to its active site depends on the drug's concentration at the receptor site. What this simply means is that, the concentration of a drug at the receptor site influences the effects of the drug.
The binding of a drugs or ligand to a receptor is purely governed by the law of mass action which states that:
The rate of the chemical reaction is directly proportional to the product of the activities or concentrations of the reactants
The higher the concentration of the drug, the greater the effects. But repeated usage can lead to a condition known as tolerance. Tolerance is simply a situation where there is a decreased response of the body to a particular type of drug due to repeated usage. Been tolerant to a drug means that you have either abused the drug or overused it. Drugs that are commonly associated with tolerance are the opiods and alcohols.
These drugs induce the hepatic enzyme - cytochrome P450 leading to accelerated metabolism of the drugs. What happens when you are tolerant to a drug is that, you will need higher dose of that same drug to produce same effect subsequently.
It is also possible to develop resistance to a drug. Resistance to a drug usually happens when you do not take a complete dosage of drug, thus allowing the microorganisms to adapt and withstand the previous destructive effect by the drug. This usually occurs mostly with antibiotics.
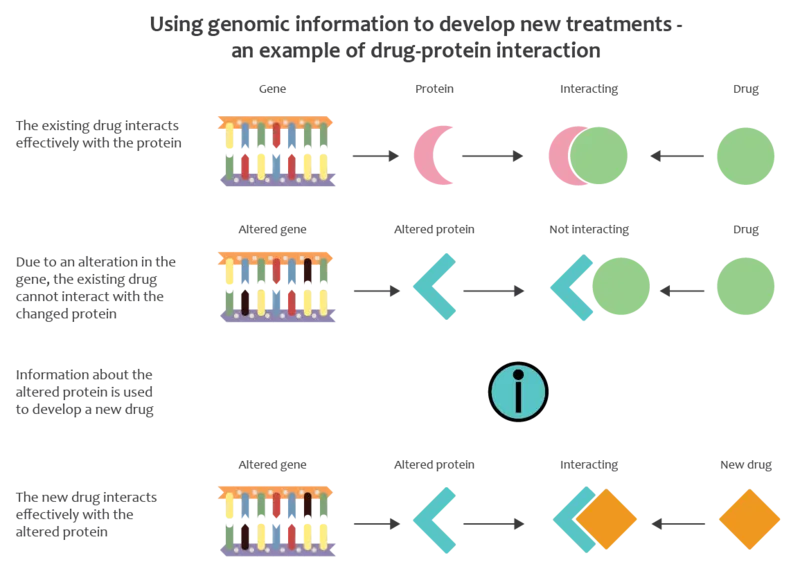
The role of pharmacogenomics in drug resistant
Pharmacogenomics is simply the study of how our gene or genetic make up affects how different individuals respond to drugs. The way you react or respond to a drug can at times vary from another person. Reason being that, your genome (all your genetic make up) varies from another person. The gene determines the type of protein you express.
All receptor are made up of protein which are product of gene. In a situation where there is an alterations or mutation in the gene that codes for receptor protein, this automatically leads to deformation in the protein molecular structure or production of abnormal receptors, thus leading to abnormal or ineffective functions of the receptor. This results to inability of the receptor to bind to drugs that would on a normal bind without resistance.
Genetic mutation or diseases can cause drugs receptor to become resistant to drugs and the best way to check this, is through the study of pharmacogenomics. Always bear in mind that, the way you respond to a drug always and most times differ from others. Even identical twins can react differently to drugs not minding that they are identical.
Of a truth, identical twins come from the same fertilized egg. For the fact that they share similar genetic profile does not make them identical in genetic make up. Identical twins are apparently not genetically identical.
Back to our discussion on receptors!
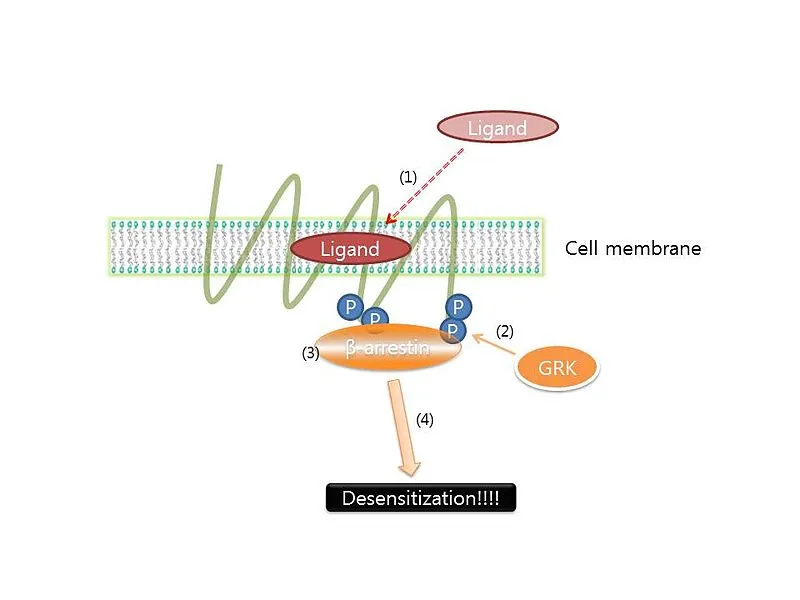
Receptors exhibit a unique phenomenon of becoming unresponsive or insensitive to drug. This phenomenon is known as tachyphylaxis. Let's briefly talk about it.
Desensitization and Tachyphylaxis
Have you ever noticed that, at some point, when you continually take a medication, it suddenly doesn't produce those severe side effects on you when compared to the initial first time you took the drug. If you continually take the drug, you would observe that there is a continuous reduction in the effects and at some point, you won't feel the effects any longer.
Your inability to feel the effects is a sort of protective mechanism by the drug receptors to avoid its damage. This is known as tachyphylaxis. By definition, tachyphylaxis also known as desensitization or refractoriness is the decreased, insensitive or unresponsive state of a drug receptor due to continuous stimuli it receives from drugs or due to the drug continuous administration.
Receptors employ this mechanism to ensure that there is no damage to its components. In a nutshell, It is a decreased biological response to a drug when given continuously. A drug administrated continues to exert it action until at a point where it begins to decline in action. A close look at the dose-response curve below says it all. You would observe there was a gradual increase in the pharmacological effect of the drug starting from point a until it reaches it's maximal pointb after which it begins to decline in potency.
Tachyphylaxis is one of the problem encountered when a drug is expected to be continually administered or when they liable and susceptible to easy degradation by liver enzymes. So since this is a major challenge in drug administration , what then is the way forward? Well the solution is not far fetched, thanks to advancement in drug discovery and the technology associated with it.
Rather than excessive administration of a particular drug, they could actually be made to stay longer and exert their therapeutic effects. This leads us to the discovery of pharmacokinetic enhancers.
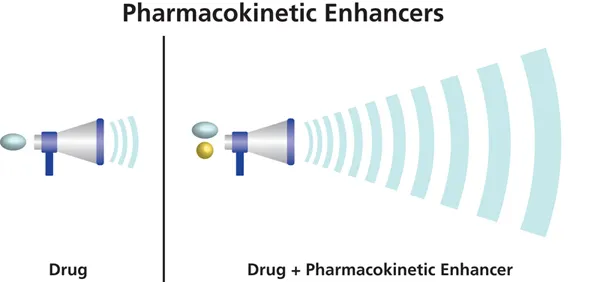
Advent of novel pharmacokinetic drug enhancers
You may no longer have to worry much about continually loading those pack of drugs in a bid to get cured of an ailment or worried about the easy degradation of drug by the liver enzymes. Pharmacokinetic enhancers come in handy especially when a drug is easily metabolised (degraded by liver enzymes - the cytochrome family of enzymes) thus the need for continuous administration of the drug but bearing in mind that at some point, the receptors will activate their protective mechanism - tachyphylaxis.
Mechanism of action of pharmacokinetic enhancers
Pharmacokinetic enhancers are a class of drugs regarded as boosters. They help to boost the therapeutic potential of another's drug. They are always given together with the drug of choice. Upon administration, the pharmacokinetic enhancer operates by interfering or blocking the breakdown of the other drug (especially those that are prone to quick or fast degradation by the liver enzymes).
Because the main or primary drug has been inhibited from quick or undesired degradation, this allows it to remain in the body at longer period and at higher concentration thus, enabling them to fully exert their therapeutic action. A good example where this drug is used is in HIV treatment regimen. Typical example of a pharmacokinetic enhancer is the Cobicistat (commonly called Tybost). It is a CYP3A inhibitor basically used to enhance the systemic exposure of the HIV drugs - atazanavir or darunavir.
With pharmacokinetic enhancers, drugs especially HIV drugs stay longer and are much effective and are able to evade degradation by the liver enzymes. Let's go into the second components of Pharmacodynamics
After the binding of drugs, events that occur afterwards are regarded as post receptor effects. Receptor must be available and free before a ligand can bind to them. Just like we earlier established from the law of mass action, the more the receptors are occupied by a ligand or a drug, the greater their Pharmacodynamic effects. This concept is what is referred to as receptor occupancy.
This though doesn't necessarily mean that all the receptor sites must be occupied before a maximum effects is obtained. Some use signal amplification to get a maximal effect thus sparring some receptor sites. This concept is what is know as spare receptors.
Note that, a drug's Pharmacodynamic effects can be altered or affected due to diseases like genetic mutation, Parkinson's disease, thyrotoxicosis (inflammation of the thyroid gland), myasthenia gravis, and even some type of insulin resistant diabetes mellitus (type 2 diabetes) etc. Aging and the competition of other drugs for the active site of a receptor can also alter the drugs pharmacodynamic effects.
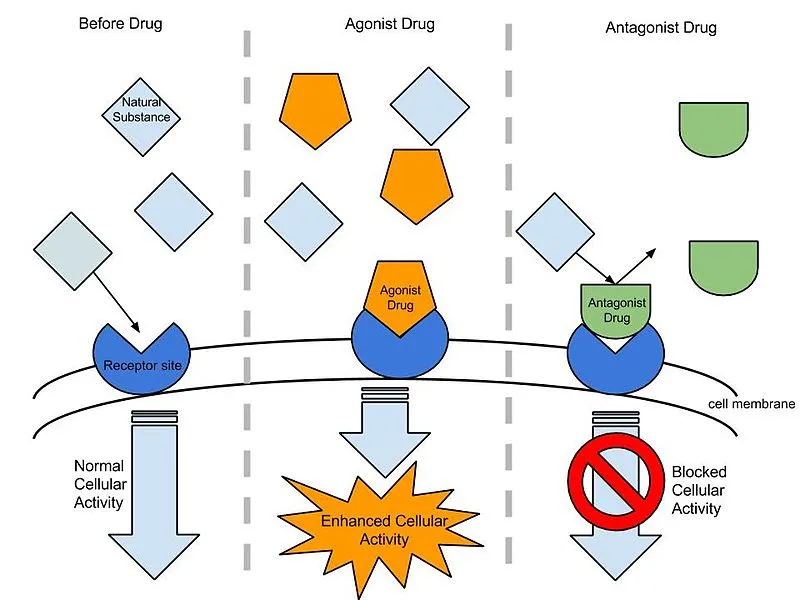
Drugs that inhibit other drugs during competition for the binding site on a receptor are generally referred to as Antagonist while those that promote binding are called Agonist. Antagonist are also referred to as inhibitors while agonist are referred to as promoters.
In a situation where two drugs compete for the same active site of a receptor, it leads to what is referred to as competitive inhibition of lesser active drug that is unable to effectively compete. This is why some drug combination are not always recommended. You can read this article for more details about drug synergism and notable combinations of drugs you should never try.
The Up and Down regulations of receptors
In a situation where there is a chronic or continuous and increased exposure of a receptor to a ligand or drugs that acts as an antagonist (has inhibitory function), this results to an upregulation (increase) in the number of the receptors but when the receptor is exposed to an Agonist (promoter), it results to a downregulation or decrease in the receptor numbers on the cell membranes.
Take the insulin receptors for example, when they are exposed to Insulin for a very long time and continuously, it leads to a gradual decrease in their number by the process of receptor internalization and degradation which is caused by increased hormonal binding. This means that over-reactivity of the islet of Langerhans that produces insulin can cause gradual damage to the Insulin receptor and this consequently results to type 2 insulin resistant diabetes mellitus.
The above does not actually apply in all cases because the nicotinic receptor acts otherwise. In cases of chronic exposure to agonists (nicotine), rather than donwregulation, there is an upregulation of the nicotinic receptors. This explains why the intake of nicotine is addictive in nature. The more you are exposed to them, the more you wish to take them.
Why aged people are predisposed to type two diabetes
As we age, there is gradual decline and alterations in the receptor binding and post receptor response sensitivity. The way your body receptor respond to drugs at young and adult stage diminishes as you grow older and it reaches a point where the receptors are no longer sensitive.
A typical example of this is seen in insulin resistant type 2 diabetes mellitus, where the insulin receptors are no longer sensitive to insulin because there has been a physiologic alterations in the receptor binding ability as well as their response sensitivity. Though other factors like overweight or obesity, sedentary life style, high intake of calories etc can also make the insulin receptors insensitive to insulin.
The chemical interaction of a drug could either produces a very serious unwanted side effects. This usually occurs when some drugs are taken concurrently with other drugs. Some could alter the effective absorption or metabolism of the primary drug while some may end up enhancing the therapeutic potency and efficacy of the primary drug. Some may not need to compete for receptors with the primary drug.
It is needful at this point to say that, not all drugs necessarily require receptor binding before they exert their therapeutic effects. Some drugs are able to produce some effects without even altering or changing any cellular function of the biological system. Some are also able to exert effects without binding to receptors.
A typical example is the mechanism of action of most antacids (drugs used for the treatment of ulcers). These drugs are bases and they reduce the acidity of the stomach by simple reaction with the acid to produce a neutral salts.
In a nutshell, what we are trying to establish here is that, the action of drugs could be direct or indirect (binding to receptors or enzymes) and immediate or delayed (neuromuscular blocking agents or those that interfere with DNA synthesis).
In conclusion, pharmacodynamics helps us determine the dose response about drugs. How they interact with the biological system of the body, their potency, max concentration and their interaction with others drugs and molecules. Always remember, the Pharmacodynamics of a drug is dependent on its binding to biological targets or its interaction and concentration at the binding site.
References
•Pharmacokinetic enhancers •Pharmacology of receptors •Pharmacokinetic Enhancers (Boosters)—Escort for Drugs against Degrading Enzymes and Beyond •Role of Pharmacokinetic enhancers in HIV therapy •Wikipedia- Pharmacodynamics •Insulin resistance •Wikipedia -diabetes in older people •Pharmacodynamics •Pharmacogenomics •Clinical pharmacologic - factors affecting response to drugs/tolerance and resistance •Drug Interactions—Principles, Examples and Clinical Consequences •Drug interaction •The Claim: Identical Twins Have Identical DNA
Return from The Pharmacodynamics of drugs - drug actions on biological system to cyprianj's Web3 Blog